654
Hormonal heaven and hell: where do the hormones
Dental hormoneWhat is the hormones, everything is more or less present. Until recently it was assumed that they are synthesized by endocrine glands or specialized endocrine cells scattered throughout the body and combined into the diffuse endocrine system. Cells of the diffuse endocrine system develop from the same germ layer, and nervous, therefore referred to as neuroendocrine. Where they are not only found in the thyroid gland, the adrenal medulla, the hypothalamus, pineal gland, placenta, pancreas and gastrointestinal tract. And recently they were found in the pulp of the tooth, and it appeared that the number of neuroendocrine cells in it varies depending on dental health.
The honor of this discovery belongs to Alexander Vladimirovich Moscow, associate Professor of Department of orthopedic stomatology of the Medical Institute of the Chuvash state University. I. N. Ulyanov. Neuroendocrine cells have characteristic proteins, and to reveal immunological methods. So A.V. Moscow who found them. (This research was published in No. 9 of the "Bulletin of experimental biology and medicine" in 2007.)
Seventy seven million eight hundred sixty six thousand five hundred ninety one
Pulp — soft serdtsevini of the tooth which contains the nerves and blood vessels. Her extracted teeth and prepared slices, which are then searched for specific proteins of the neuroendocrine cells. Did it in three stages. First, the prepared sections were treated with antibodies to the target proteins (antigens). Antibodies consist of two parts: specific and nonspecific. After binding with antigens, they remain non-specific on the cut part up. Slice treated with antibodies to this non-specific parts, which are marked with Biotin. Then this "sandwich" with Biotin from top treated with a special reagent, and the localization of the source of the protein appears as a reddish spot.
Neuroendocrine cells differ from connective tissue cells and larger size, irregular shape and the presence in the cytoplasm reddish-brown clumps (colored proteins), often covering the nucleus.
In a healthy pulp neuroendocrine cells a little, but caries the number is growing. If the tooth is not treated, the disease progresses, and neuroendocrine cells becomes more and more, and they accumulate around the lesion. The peak of their strength it is necessary to tooth decay so neglected, that become inflamed and the tissues around the tooth, then there is periodontitis.
For patients who prefer long to suffer at home than to go to the doctor, the inflammation of the pulp and periodontium. At this stage the number of neuroendocrine cells is reduced (although still higher than in healthy pulp) — they are superseded by inflammatory cells (leukocytes and macrophages). Reduces their numbers and chronic pulpitis, but in this disease the cells in the pulp generally stays small, they are replaced by sclerotic bands.
According to A. V. Moscow, neuroendocrine cells of dental caries, pulpitis regulate in the area of inflammation microcirculation and metabolism. Because of nerve fibers in dental caries, pulpitis becomes more endocrine and nervous system and in this regard work together.
Hormones everywhere?In recent years, scientists found that hormone production is not the prerogative of specialised endocrine cells and glands. Doing this and other cells, which have many other tasks. Their list grows from year to year. It has got various blood cells (lymphocytes, eosinophils, monocytes and platelets), crawling out of the blood vessels, macrophages, endothelial cells (lining blood vessels), and epithelial cells of the thymus, chondrocytes (cartilage), cells of the amniotic fluid and placental trophoblast (the part of the placenta, which grows into the uterus) and the endometrium (from the womb), Leydig cells of the testes, some retinal cells and the cells of the Mer-fect located in the skin around the hair and in the epithelium of the subungual bed, muscle cells. The list of synthesized hormones that they are also quite long.
Take, for example, lymphocytes of mammals. In addition to the nominal production of the antibody they synthesize melatonin, prolactin, ACTH (adrenocorticotropic hormone) and growth hormone. "Homeland" melatonin is traditionally believed the pineal gland — gland located in the human brain. It is synthesized and cells of the diffuse neuroendocrine system. Action spectrum of melatonin broad: it regulates biorhythms (the particularly famous), the differentiation and cell division, inhibits the growth of some tumors and stimulates the production of interferon. Prolactin, which causes lactation, produces the anterior lobe of the pituitary, but in lymphocytes it acts as a growth factor for cells. ACTH, which is synthesized in the anterior pituitary gland, stimulates the synthesis of steroid hormones of the adrenal cortex and in lymphocytes regulates the formation of antibodies.
And the cells of the thymus, the organ in which are formed T-lymphocytes that synthesize luteinizing hormone (the pituitary hormone that causes testosterone synthesis in the testes and estrogen in the ovaries). In the thymus it apparently stimulates cell division.
The hormone synthesis in lymphocytes and thymus cells many experts consider as proof of the existence of a link between the endocrine and immune systems. But it is also a very significant illustration of the current state of endocrinology: it is impossible to say that a hormone is synthesized there and makes something. Its sites of synthesis can be a lot of features too, and they often depend on the place of education hormone.
Endocrine layerSometimes congestion nonspecific hormoneproducing cells form a full-fledged endocrine organ, and rather big, such as fat tissue. However, its dimensions are variable, and depending on them change the range of "fat" hormones and their activity.
Fat, delivering modern man so much trouble, really is a valuable evolutionary acquisition.
In the 1960-ies the American geneticist James Neal has formulated the hypothesis of the "Thrifty genes". According to this hypothesis, early human history, and not only for early, typical periods of extended starvation. Survived those between the hungry years time to fatten up to then was to lose weight. Therefore, evolution selected alleles that contributed to rapid weight gain and declined person-to-low mobility — sidyuchi, fat is not stomping. (Genes that affect the behaviors and development of obesity, has been known for several hundred.) But life has changed and these stores now we are not for the future, and to disease. The excess fat causes a grave disease and metabolic syndrome: combination of obesity, resistance to insulin, high blood pressure and chronic inflammation. The patient with metabolic syndrome not long to wait for cardiovascular diseases, type II diabetes and many other ailments. And all this is the result of adipose tissue as an endocrine organ.
The main cells of adipose tissue, adipocytes, it is not similar to the secretory cells. However, they do not only store fat but also secrete hormones. Chief among them, adiponectin, prevents the development of atherosclerosis and General inflammation. It affects the signal from the insulin receptor and thereby prevents the formation of insulinrezistentnost. Fatty acids in muscle cells and the liver under its influence oxidize faster, active forms of oxygen becomes less, and diabetes, if it is already there, it flows easier. Moreover, adiponectin regulates the function of the adipocytes themselves.
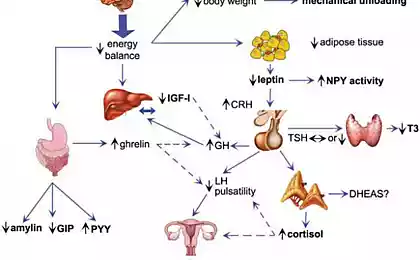
Another great adipose tissue hormone — leptin. As adipokinetic, it is synthesized by the adipocytes. Leptin is known that suppresses the appetite and accelerates the oxidation of fatty acids. Such an effect he achieves by interacting with certain neurons of the hypothalamus and then hypothalamus disposes. When excess body weight production of leptin increases significantly, and the hypothalamic neurons reduces sensitivity to it, and the hormone is haunting blood unrelated. Therefore, although leptin levels in the serum of patients with obesity increased, people do not lose weight because the hypothalamus it signals does not accept. However, the receptors for leptin in other tissues, their sensitivity to the hormone remains the same, and they are willing to respond to his signals. And leptin, among other things, activates the sympathetic division of the peripheral nervous system and increases blood pressure, stimulates inflammation and promotes the formation of blood clots, in other words, making a strong contribution to the development of hypertension and inflammation characteristic of metabolic syndrome.It would seem that the essential adiponectin in obesity and can prevent the development of metabolic syndrome. But, alas, the stronger grows fat tissue, the less of the hormone it produces. Adiponectin is present in the blood in the form of trimers and hexamers. When obesity becomes more of trimers and hexamers is less, although hexamers much better interact with cell receptors. And the number of receptors in the growth of adipose tissue is reduced. So the hormone is not just getting smaller, he is also acting weaker, which, in turn, contributes to the development of obesity. It is a vicious circle. But it can be broken — to lose weight pounds at 12, is not less then the number of receptors returns to normal.
The development of inflammation and insulin resistance also causes another hormone of adipocytes, resistin. The resistin is an insulin antagonist, under the action of the heart muscle cells reduces glucose consumption and accumulate intracellular fat. And adipocytes under the influence of resistin is synthesized much more inflammatory factors: chemotactic for macrophages protein 1, interleukin-6 and tumor necrosis factor-b (MCP-1, IL-6 and TNF-b). The more resistin in the serum, the higher systolic pressure, a wider waist, more the risk of developing cardiovascular disease.
In fairness it should be noted that the expanding adipose tissue tends to repair the damage caused by her hormones. To this end, the adipocytes of patients with obesity in excess produce two hormones: visfatin and apelin. However, their synthesis occurs in other organs, including skeletal muscle and liver. In principle, these hormones oppose the development of metabolic syndrome. Visfatin acts like insulin (binds to insulin receptor), and reduces the level of glucose in the blood, and even in a very complex manner activates the synthesis of adiponectin. But certainly useful this hormone cannot be called because visfatin stimulates the synthesis of the signals of inflammation. Apelin inhibits insulin secretion by binding to receptors of the beta cells of the pancreas, lowers blood pressure, stimulates the contraction of heart muscle cells. When reducing the mass of adipose tissue content in the blood is reduced. Unfortunately, apelin and visfatin can't resist adiposity effects of other hormones.
Skeletal the hormones
Hormonal activity of adipose tissue explains why excess weight leads to such serious consequences. However, scientists have recently discovered in mammals endocrine organ larger. It turns out that our skeleton produces at least two hormones. One regulates mineralization of bones, the other the sensitivity of cells to insulin.Skeletal the hormones.
Bone takes care of itselfReaders of "Chemistry and life" know that bone is alive. Osteoblasts build it. These cells synthesize and secrete large amounts of proteins, mainly collagen, osteocalcin and osteopontin, creating organic matrix of bone that is then mineralized. During mineralization the calcium ions are associated with inorganic phosphate to form hydroxyapatite [Ca10(PO)4(OH)2]. Surrounding himself with mineralized organic matrix, osteoblasts become osteocytes — Mature, mnogochastichnye spindle-shaped cells with large rounded nucleus and a small amount of organelles. The osteocytes do not come into contact with calzinirovnie matrix, between them and the walls of their "caves" there is a gap width of about 0.1 µm, and the walls themselves are lined with a thin, 1-2 µm, layer demineralizovannoj tissue. The osteocytes are connected to each other by long processes extending at the special tubules. On the same tubules and vesicles around the osteocytes circulates the interstitial fluid, feeding cells.
Bone mineralization proceeds normally subject to several conditions. First of all you need a certain concentration of calcium and phosphorus in the blood. These elements come from food through the intestine and out with the urine. Therefore, the kidneys, the filtering the urine, have to hold ions of calcium and phosphorus in the body (this is called reabsorption).
Proper absorption of calcium and phosphorus in the intestine provides the active form of vitamin D (calcitriol). It also affects the synthetic activity of osteoblasts. Vitamin D is transformed into calcitriol by the enzyme 1B-hydroxylase, which is synthesized mainly in the kidneys. Another factor affecting the level of calcium and phosphorus in blood and the activity of osteoblasts, parathyroid hormone (PTH), a product of the parathyroid glands. PTG interacts with bone, kidney and intestinal tissues and reduces reabsorption.
But recently, scientists have discovered another factor regulating the mineralization of bones — protein FGF23, fibroblast growth factor 23. (Great contribution to this work made by the employees of pharmaceutical research lab brewing company "Kirin" and the Department of Nephrology and endocrinology, University of Tokyo under the guidance of Takahasi Yamashita. Synthesis occurs FGF23 in osteocytes, and he acts on the kidneys, controlling the level of inorganic phosphate and calcitriol.
As found by Japanese scientists, the gene FGF23 (hereinafter genes, unlike their proteins are indicated in italics) responsible for two serious diseases: autosomal dominant hypophosphatemic rickets and osteomalacia. Put simply, the rickets is a violation of mineralization of the growing bones of children. And the word "gipofosfatemia" means that the disease is caused by a lack of phosphate in the body. Osteomalacia is demineralization (softening) of bones in adults caused by lack of vitamin D. patients suffering From these diseases, increased levels of FGF23 protein. Sometimes osteomalacia occurs as a result of tumor development, and not bone. In the cells of these tumors also increased expression of FGF23.
All patients with FGF23 overproduction reduced the content of phosphorus in the blood and renal reabsorption weakened. If these processes were under the control of PTH, the violation of phosphorus metabolism would entail increased formation of calcitriol. But this is not happening. In osteomalacia both species the concentration of calcitriol in the serum remains low. Therefore, in the regulation of phosphorus metabolism in these diseases the first violin plays PTH, and FGF23. As scientists discovered this enzyme suppresses the synthesis of 1B-hydroxylase in the kidney, therefore, there is a lack of active form of vitamin D.
With a lack of FGF23, the picture is reversed: phosphorus in the blood in excess, calcitriol is also. A similar situation occurs in mutant mice with increased levels of protein. And in rodents with a missing gene FGF23 is the opposite: hyperphosphaturia, increased renal phosphate reabsorption, high levels of calcitriol, and increased expression 1B-hydroxylase. As a result, the researchers came to the conclusion that FGF23 regulates phosphate metabolism vitamin D, and this path of regulation is different from the previously known ways of involving PTH.
The mechanisms of action of FGF23 scientists now understand. It is known that it reduces the expression of proteins responsible for the uptake of phosphate in the renal tubules, as well as экспрессию1б-hydroxylase. Because FGF23 is synthesized by osteocytes and acts on kidney cells, getting there through the blood, this protein can be called a classic hormone, although the bone no one would dare to name the endocrine gland.
Levels of the hormone depends on the content of phosphate ions in the blood, and mutations in certain genes that affect mineral metabolism (FGF23're not the only gene with such function), and mutations in the gene. This protein, like any other, is in the blood for a certain time, and then cleaved by special enzymes. But if the result of a mutation of the hormone acquires resistance to splitting, it will be too much. And then there is the GALNT3 gene, the product of which cleaves FGF23 protein. Mutation in this gene causes increased breakdown of the hormone and a normal level of synthesis the patient lacks FGF23 with all the ensuing consequences. KLOTHO protein is required for interaction of the hormone with the receptor. And somehow FGF23 interacts with PTG, of course. The researchers suggest that it inhibits the synthesis of parathyroid hormone, but not so sure. But scientists continue to work and soon, apparently, make out all of the action and interaction of FGF23 to the last bone. Wait.
The skeleton and diabetesprone should mineralization of bones is impossible without the maintenance of normal levels of calcium and phosphate in serum. It is therefore quite understandable that bone "personally" controls these processes. But what does she, one wonders, to the sensitivity of cells to insulin? However, in 2007, researchers from Columbia University (new York), led by Gerard Karsenty discovered, to the amazement of the scientific community that the sensitivity of cells to insulin is affected by osteocalcin. This, as we remember, one of the key proteins of the bone matrix, the second value after the collagen and osteoblasts synthesize it. Immediately after the synthesis of a special enzyme carboxylase three residue glutamic acid osteocalcin, that is, introduces them to a carboxyl group. In this form of osteocalcin and included in bone. But part of protein molecules remains decarbauxilirovanie. Such osteocalcin indicate uOCN, he has hormonal activity. The process of carboxylation of osteocalcin enhances osteoarticulares protein tyrosinosis (OST-PTP), reducing, thus, the activity of the hormone uOCN.
It began with the fact that American scientists have created a line of "biosteering" mice. The synthesis of the bone matrix such animals have passed with more speed than normal, so the bones were more massive, but its functions have performed well. In these mice, the researchers found hyperglycemia, low insulin levels, reduced number and a reduced activity of the insulin-producing beta cells of the pancreas and increased content of visceral fat. (Fat is subcutaneous and visceral, pending in the abdominal cavity. The amount of visceral fat depends mostly on diet, not on the genotype.) But in mice deficient in the gene OST-PTP, that is, with excessive activity uOCN, the clinical picture is the opposite: too much beta-cells and insulin sensitivity of cells to insulin, hypoglycemia, fat is almost there. After injection uOCN in normal mice increases the number of beta cells, the activity of the insulin synthesis and sensitivity to it. The glucose level comes to normal. So uOCN is a hormone that is synthesized in the osteoblasts, acts on cells in the pancreas and muscle cells. And it affects on insulin production and sensitivity to it, respectively.
All this is set on the mice, but what about men? According to the few clinical studies, the level of osteocalcin is positively associated with insulin sensitivity and in the blood of diabetics was significantly lower than that of people not suffering from this disease. However, in these studies, physicians did not distinguish between carboxylated osteocalcin and decarbauxilirovanie. What is the role of these forms of protein in the human body have yet to understand.
But what is the role of the skeleton, it turns out! And we thought that this was a support for muscles.
FGF23 and osteocalcin — classic hormones. They are synthesized in one organ and affect the others. However, their example shows that the synthesis of hormones don't always have the specific function of selected cells. Rather, it is biological and inherent in any living cell, regardless of its primary role in the body.
It's interesting: Hormones of well-being
Erased not only the distinction between endocrine and endokrinnye cells, the concept of "hormone" has become increasingly blurred. For example, adrenaline, dopamine and serotonin, of course, the hormones, but they are also neurotransmitters, acting for and through the blood, and through the synapse. And adiponectin has not only endocrine, but also paracrine, that is, acts not only through the blood into distant organs, but also through the interstitial fluid to neighboring cells of adipose tissue. So the subject of endocrinology is changing. published
Author :Natalia Lvovna Reznik, candidate of biology
Watch the video on the Chemistry of the body. Hormonal Hormonal hell and Paradise
Put LIKES and share with your FRIENDS!
www.youtube.com/channel/UCXd71u0w04qcwk32c8kY2BA/videos
Subscribe -https://www.facebook.com//
P. S. And remember, only by changing their consumption — together we change the world! ©
Source: elementy.ru/nauchno-populyarnaya_biblioteka/431294/Otkuda_berutsya_gormony
The honor of this discovery belongs to Alexander Vladimirovich Moscow, associate Professor of Department of orthopedic stomatology of the Medical Institute of the Chuvash state University. I. N. Ulyanov. Neuroendocrine cells have characteristic proteins, and to reveal immunological methods. So A.V. Moscow who found them. (This research was published in No. 9 of the "Bulletin of experimental biology and medicine" in 2007.)
Seventy seven million eight hundred sixty six thousand five hundred ninety one
Pulp — soft serdtsevini of the tooth which contains the nerves and blood vessels. Her extracted teeth and prepared slices, which are then searched for specific proteins of the neuroendocrine cells. Did it in three stages. First, the prepared sections were treated with antibodies to the target proteins (antigens). Antibodies consist of two parts: specific and nonspecific. After binding with antigens, they remain non-specific on the cut part up. Slice treated with antibodies to this non-specific parts, which are marked with Biotin. Then this "sandwich" with Biotin from top treated with a special reagent, and the localization of the source of the protein appears as a reddish spot.
Neuroendocrine cells differ from connective tissue cells and larger size, irregular shape and the presence in the cytoplasm reddish-brown clumps (colored proteins), often covering the nucleus.
In a healthy pulp neuroendocrine cells a little, but caries the number is growing. If the tooth is not treated, the disease progresses, and neuroendocrine cells becomes more and more, and they accumulate around the lesion. The peak of their strength it is necessary to tooth decay so neglected, that become inflamed and the tissues around the tooth, then there is periodontitis.
For patients who prefer long to suffer at home than to go to the doctor, the inflammation of the pulp and periodontium. At this stage the number of neuroendocrine cells is reduced (although still higher than in healthy pulp) — they are superseded by inflammatory cells (leukocytes and macrophages). Reduces their numbers and chronic pulpitis, but in this disease the cells in the pulp generally stays small, they are replaced by sclerotic bands.
According to A. V. Moscow, neuroendocrine cells of dental caries, pulpitis regulate in the area of inflammation microcirculation and metabolism. Because of nerve fibers in dental caries, pulpitis becomes more endocrine and nervous system and in this regard work together.
Hormones everywhere?In recent years, scientists found that hormone production is not the prerogative of specialised endocrine cells and glands. Doing this and other cells, which have many other tasks. Their list grows from year to year. It has got various blood cells (lymphocytes, eosinophils, monocytes and platelets), crawling out of the blood vessels, macrophages, endothelial cells (lining blood vessels), and epithelial cells of the thymus, chondrocytes (cartilage), cells of the amniotic fluid and placental trophoblast (the part of the placenta, which grows into the uterus) and the endometrium (from the womb), Leydig cells of the testes, some retinal cells and the cells of the Mer-fect located in the skin around the hair and in the epithelium of the subungual bed, muscle cells. The list of synthesized hormones that they are also quite long.
Take, for example, lymphocytes of mammals. In addition to the nominal production of the antibody they synthesize melatonin, prolactin, ACTH (adrenocorticotropic hormone) and growth hormone. "Homeland" melatonin is traditionally believed the pineal gland — gland located in the human brain. It is synthesized and cells of the diffuse neuroendocrine system. Action spectrum of melatonin broad: it regulates biorhythms (the particularly famous), the differentiation and cell division, inhibits the growth of some tumors and stimulates the production of interferon. Prolactin, which causes lactation, produces the anterior lobe of the pituitary, but in lymphocytes it acts as a growth factor for cells. ACTH, which is synthesized in the anterior pituitary gland, stimulates the synthesis of steroid hormones of the adrenal cortex and in lymphocytes regulates the formation of antibodies.
And the cells of the thymus, the organ in which are formed T-lymphocytes that synthesize luteinizing hormone (the pituitary hormone that causes testosterone synthesis in the testes and estrogen in the ovaries). In the thymus it apparently stimulates cell division.
The hormone synthesis in lymphocytes and thymus cells many experts consider as proof of the existence of a link between the endocrine and immune systems. But it is also a very significant illustration of the current state of endocrinology: it is impossible to say that a hormone is synthesized there and makes something. Its sites of synthesis can be a lot of features too, and they often depend on the place of education hormone.
Endocrine layerSometimes congestion nonspecific hormoneproducing cells form a full-fledged endocrine organ, and rather big, such as fat tissue. However, its dimensions are variable, and depending on them change the range of "fat" hormones and their activity.
Fat, delivering modern man so much trouble, really is a valuable evolutionary acquisition.
In the 1960-ies the American geneticist James Neal has formulated the hypothesis of the "Thrifty genes". According to this hypothesis, early human history, and not only for early, typical periods of extended starvation. Survived those between the hungry years time to fatten up to then was to lose weight. Therefore, evolution selected alleles that contributed to rapid weight gain and declined person-to-low mobility — sidyuchi, fat is not stomping. (Genes that affect the behaviors and development of obesity, has been known for several hundred.) But life has changed and these stores now we are not for the future, and to disease. The excess fat causes a grave disease and metabolic syndrome: combination of obesity, resistance to insulin, high blood pressure and chronic inflammation. The patient with metabolic syndrome not long to wait for cardiovascular diseases, type II diabetes and many other ailments. And all this is the result of adipose tissue as an endocrine organ.
The main cells of adipose tissue, adipocytes, it is not similar to the secretory cells. However, they do not only store fat but also secrete hormones. Chief among them, adiponectin, prevents the development of atherosclerosis and General inflammation. It affects the signal from the insulin receptor and thereby prevents the formation of insulinrezistentnost. Fatty acids in muscle cells and the liver under its influence oxidize faster, active forms of oxygen becomes less, and diabetes, if it is already there, it flows easier. Moreover, adiponectin regulates the function of the adipocytes themselves.
Another great adipose tissue hormone — leptin. As adipokinetic, it is synthesized by the adipocytes. Leptin is known that suppresses the appetite and accelerates the oxidation of fatty acids. Such an effect he achieves by interacting with certain neurons of the hypothalamus and then hypothalamus disposes. When excess body weight production of leptin increases significantly, and the hypothalamic neurons reduces sensitivity to it, and the hormone is haunting blood unrelated. Therefore, although leptin levels in the serum of patients with obesity increased, people do not lose weight because the hypothalamus it signals does not accept. However, the receptors for leptin in other tissues, their sensitivity to the hormone remains the same, and they are willing to respond to his signals. And leptin, among other things, activates the sympathetic division of the peripheral nervous system and increases blood pressure, stimulates inflammation and promotes the formation of blood clots, in other words, making a strong contribution to the development of hypertension and inflammation characteristic of metabolic syndrome.It would seem that the essential adiponectin in obesity and can prevent the development of metabolic syndrome. But, alas, the stronger grows fat tissue, the less of the hormone it produces. Adiponectin is present in the blood in the form of trimers and hexamers. When obesity becomes more of trimers and hexamers is less, although hexamers much better interact with cell receptors. And the number of receptors in the growth of adipose tissue is reduced. So the hormone is not just getting smaller, he is also acting weaker, which, in turn, contributes to the development of obesity. It is a vicious circle. But it can be broken — to lose weight pounds at 12, is not less then the number of receptors returns to normal.
The development of inflammation and insulin resistance also causes another hormone of adipocytes, resistin. The resistin is an insulin antagonist, under the action of the heart muscle cells reduces glucose consumption and accumulate intracellular fat. And adipocytes under the influence of resistin is synthesized much more inflammatory factors: chemotactic for macrophages protein 1, interleukin-6 and tumor necrosis factor-b (MCP-1, IL-6 and TNF-b). The more resistin in the serum, the higher systolic pressure, a wider waist, more the risk of developing cardiovascular disease.
In fairness it should be noted that the expanding adipose tissue tends to repair the damage caused by her hormones. To this end, the adipocytes of patients with obesity in excess produce two hormones: visfatin and apelin. However, their synthesis occurs in other organs, including skeletal muscle and liver. In principle, these hormones oppose the development of metabolic syndrome. Visfatin acts like insulin (binds to insulin receptor), and reduces the level of glucose in the blood, and even in a very complex manner activates the synthesis of adiponectin. But certainly useful this hormone cannot be called because visfatin stimulates the synthesis of the signals of inflammation. Apelin inhibits insulin secretion by binding to receptors of the beta cells of the pancreas, lowers blood pressure, stimulates the contraction of heart muscle cells. When reducing the mass of adipose tissue content in the blood is reduced. Unfortunately, apelin and visfatin can't resist adiposity effects of other hormones.
Skeletal the hormones
Hormonal activity of adipose tissue explains why excess weight leads to such serious consequences. However, scientists have recently discovered in mammals endocrine organ larger. It turns out that our skeleton produces at least two hormones. One regulates mineralization of bones, the other the sensitivity of cells to insulin.Skeletal the hormones.
Bone takes care of itselfReaders of "Chemistry and life" know that bone is alive. Osteoblasts build it. These cells synthesize and secrete large amounts of proteins, mainly collagen, osteocalcin and osteopontin, creating organic matrix of bone that is then mineralized. During mineralization the calcium ions are associated with inorganic phosphate to form hydroxyapatite [Ca10(PO)4(OH)2]. Surrounding himself with mineralized organic matrix, osteoblasts become osteocytes — Mature, mnogochastichnye spindle-shaped cells with large rounded nucleus and a small amount of organelles. The osteocytes do not come into contact with calzinirovnie matrix, between them and the walls of their "caves" there is a gap width of about 0.1 µm, and the walls themselves are lined with a thin, 1-2 µm, layer demineralizovannoj tissue. The osteocytes are connected to each other by long processes extending at the special tubules. On the same tubules and vesicles around the osteocytes circulates the interstitial fluid, feeding cells.
Bone mineralization proceeds normally subject to several conditions. First of all you need a certain concentration of calcium and phosphorus in the blood. These elements come from food through the intestine and out with the urine. Therefore, the kidneys, the filtering the urine, have to hold ions of calcium and phosphorus in the body (this is called reabsorption).
Proper absorption of calcium and phosphorus in the intestine provides the active form of vitamin D (calcitriol). It also affects the synthetic activity of osteoblasts. Vitamin D is transformed into calcitriol by the enzyme 1B-hydroxylase, which is synthesized mainly in the kidneys. Another factor affecting the level of calcium and phosphorus in blood and the activity of osteoblasts, parathyroid hormone (PTH), a product of the parathyroid glands. PTG interacts with bone, kidney and intestinal tissues and reduces reabsorption.
But recently, scientists have discovered another factor regulating the mineralization of bones — protein FGF23, fibroblast growth factor 23. (Great contribution to this work made by the employees of pharmaceutical research lab brewing company "Kirin" and the Department of Nephrology and endocrinology, University of Tokyo under the guidance of Takahasi Yamashita. Synthesis occurs FGF23 in osteocytes, and he acts on the kidneys, controlling the level of inorganic phosphate and calcitriol.
As found by Japanese scientists, the gene FGF23 (hereinafter genes, unlike their proteins are indicated in italics) responsible for two serious diseases: autosomal dominant hypophosphatemic rickets and osteomalacia. Put simply, the rickets is a violation of mineralization of the growing bones of children. And the word "gipofosfatemia" means that the disease is caused by a lack of phosphate in the body. Osteomalacia is demineralization (softening) of bones in adults caused by lack of vitamin D. patients suffering From these diseases, increased levels of FGF23 protein. Sometimes osteomalacia occurs as a result of tumor development, and not bone. In the cells of these tumors also increased expression of FGF23.
All patients with FGF23 overproduction reduced the content of phosphorus in the blood and renal reabsorption weakened. If these processes were under the control of PTH, the violation of phosphorus metabolism would entail increased formation of calcitriol. But this is not happening. In osteomalacia both species the concentration of calcitriol in the serum remains low. Therefore, in the regulation of phosphorus metabolism in these diseases the first violin plays PTH, and FGF23. As scientists discovered this enzyme suppresses the synthesis of 1B-hydroxylase in the kidney, therefore, there is a lack of active form of vitamin D.
With a lack of FGF23, the picture is reversed: phosphorus in the blood in excess, calcitriol is also. A similar situation occurs in mutant mice with increased levels of protein. And in rodents with a missing gene FGF23 is the opposite: hyperphosphaturia, increased renal phosphate reabsorption, high levels of calcitriol, and increased expression 1B-hydroxylase. As a result, the researchers came to the conclusion that FGF23 regulates phosphate metabolism vitamin D, and this path of regulation is different from the previously known ways of involving PTH.
The mechanisms of action of FGF23 scientists now understand. It is known that it reduces the expression of proteins responsible for the uptake of phosphate in the renal tubules, as well as экспрессию1б-hydroxylase. Because FGF23 is synthesized by osteocytes and acts on kidney cells, getting there through the blood, this protein can be called a classic hormone, although the bone no one would dare to name the endocrine gland.
Levels of the hormone depends on the content of phosphate ions in the blood, and mutations in certain genes that affect mineral metabolism (FGF23're not the only gene with such function), and mutations in the gene. This protein, like any other, is in the blood for a certain time, and then cleaved by special enzymes. But if the result of a mutation of the hormone acquires resistance to splitting, it will be too much. And then there is the GALNT3 gene, the product of which cleaves FGF23 protein. Mutation in this gene causes increased breakdown of the hormone and a normal level of synthesis the patient lacks FGF23 with all the ensuing consequences. KLOTHO protein is required for interaction of the hormone with the receptor. And somehow FGF23 interacts with PTG, of course. The researchers suggest that it inhibits the synthesis of parathyroid hormone, but not so sure. But scientists continue to work and soon, apparently, make out all of the action and interaction of FGF23 to the last bone. Wait.
The skeleton and diabetesprone should mineralization of bones is impossible without the maintenance of normal levels of calcium and phosphate in serum. It is therefore quite understandable that bone "personally" controls these processes. But what does she, one wonders, to the sensitivity of cells to insulin? However, in 2007, researchers from Columbia University (new York), led by Gerard Karsenty discovered, to the amazement of the scientific community that the sensitivity of cells to insulin is affected by osteocalcin. This, as we remember, one of the key proteins of the bone matrix, the second value after the collagen and osteoblasts synthesize it. Immediately after the synthesis of a special enzyme carboxylase three residue glutamic acid osteocalcin, that is, introduces them to a carboxyl group. In this form of osteocalcin and included in bone. But part of protein molecules remains decarbauxilirovanie. Such osteocalcin indicate uOCN, he has hormonal activity. The process of carboxylation of osteocalcin enhances osteoarticulares protein tyrosinosis (OST-PTP), reducing, thus, the activity of the hormone uOCN.
It began with the fact that American scientists have created a line of "biosteering" mice. The synthesis of the bone matrix such animals have passed with more speed than normal, so the bones were more massive, but its functions have performed well. In these mice, the researchers found hyperglycemia, low insulin levels, reduced number and a reduced activity of the insulin-producing beta cells of the pancreas and increased content of visceral fat. (Fat is subcutaneous and visceral, pending in the abdominal cavity. The amount of visceral fat depends mostly on diet, not on the genotype.) But in mice deficient in the gene OST-PTP, that is, with excessive activity uOCN, the clinical picture is the opposite: too much beta-cells and insulin sensitivity of cells to insulin, hypoglycemia, fat is almost there. After injection uOCN in normal mice increases the number of beta cells, the activity of the insulin synthesis and sensitivity to it. The glucose level comes to normal. So uOCN is a hormone that is synthesized in the osteoblasts, acts on cells in the pancreas and muscle cells. And it affects on insulin production and sensitivity to it, respectively.
All this is set on the mice, but what about men? According to the few clinical studies, the level of osteocalcin is positively associated with insulin sensitivity and in the blood of diabetics was significantly lower than that of people not suffering from this disease. However, in these studies, physicians did not distinguish between carboxylated osteocalcin and decarbauxilirovanie. What is the role of these forms of protein in the human body have yet to understand.
But what is the role of the skeleton, it turns out! And we thought that this was a support for muscles.
FGF23 and osteocalcin — classic hormones. They are synthesized in one organ and affect the others. However, their example shows that the synthesis of hormones don't always have the specific function of selected cells. Rather, it is biological and inherent in any living cell, regardless of its primary role in the body.
It's interesting: Hormones of well-being
Erased not only the distinction between endocrine and endokrinnye cells, the concept of "hormone" has become increasingly blurred. For example, adrenaline, dopamine and serotonin, of course, the hormones, but they are also neurotransmitters, acting for and through the blood, and through the synapse. And adiponectin has not only endocrine, but also paracrine, that is, acts not only through the blood into distant organs, but also through the interstitial fluid to neighboring cells of adipose tissue. So the subject of endocrinology is changing. published
Author :Natalia Lvovna Reznik, candidate of biology
Watch the video on the Chemistry of the body. Hormonal Hormonal hell and Paradise
Put LIKES and share with your FRIENDS!
www.youtube.com/channel/UCXd71u0w04qcwk32c8kY2BA/videos
Subscribe -https://www.facebook.com//
P. S. And remember, only by changing their consumption — together we change the world! ©
Source: elementy.ru/nauchno-populyarnaya_biblioteka/431294/Otkuda_berutsya_gormony