642
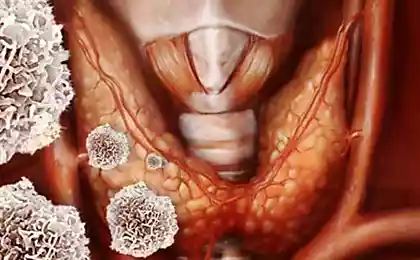
Find out the TRUTH! What are the dangers of red and processed meat
In October 2015 22 scientists from ten countries met at the International Agency for research on cancer (IARC) in Lyon (France) to assess the Carcinogenicity of consumption of raw and processed red meat. Their findings should be published in 114 volumes of the IARC monographs.
Red meat — unprocessed part of the muscles of mammals, such as beef, veal, pork, mutton, lamb, beef or goat meat, including minced meat or frozen meat; commonly used after cooking.
Processed meat — meat, prepared by salting, boiling, fermentation, Smoking or other processes to improve the taste or increase shelf life. Most often, processed meat is pork or beef, but it can also include other varieties, poultry, offal, or offal, such as liver or blood.
Red meat contains proteins of high biological value and important minerals such as b vitamins, iron (free and associated with the heme) and zinc. The fat content of red meat varies according to animal species, age, sex, breeds, feeds and parts of the carcass.
Meat processing, for example, cooking or Smoking, can lead to the formation of carcinogenic chemicals, including N-nitroso-compounds (NOC) and polycyclic aromatic hydrocarbons (PAHs).
Cooking not only improves the digestibility and palatability of meat, but may cause the formation to known or suspected carcinogens, including heterocyclic aromatic amines (haa) and PAHs. Cooking food at high temperatures via frying, grilling or barbecue, in General, produces the greatest number of these compounds.
The average level of consumption of red meat among ordinary consumers is about 50-100 g per person per day, with a high level of consumption is estimated at more than 200 g per person per day.
The consumption of processed meat available information less. The working group assessed more than 800 epidemiological studies examining the correlation of cancer incidence with the consumption of red or processed meat in many countries on several continents, and involving the various ethnic groups and diets.
The most significant for the evaluation was a prospective cohort study conducted in the General population. High-quality sampling study on the basis of the General population provide additional evidence.
In drafting both those, and others, considered to be the most informative studies were those that considered separately the consumption of red and processed meat, had quantitative information on diet is obtained from the verified questionnaire, a large sample size and controlled for the major potential confounders (confounding factors, approx. ed.) relating to the location of the tumor.

The largest array of epidemiological data for colorectal cancer. Data on the correlation of consumption of red meat with colorectal cancer were obtained from 14 cohort studies. A positive correlation was observed at high levels of consumption of red meat (compared to low) in half of these studies, including cohort study based on a sample of residents of ten European countries, covering a wide range of meat consumption, as well as other large cohort studies from Sweden and Australia.
Of the 15 considered informative research method case-control, seven reported a positive correlation of colorectal cancer with high consumption of red meat (compared with lowest consumption level). Positive correlation of this disease with the consumption of processed meat was found in 12 of the 18 cohort studies that provided relevant data, including studies in Europe, Japan and the United States.
Supporting data came from six of the nine informative research method “case-control”. A meta-analysis of ten cohort studies of colorectal cancer reported a statistically significant relationship “dose-response”, with a 17% increased risk (95% CI (confidence interval) of 1.05 to 1.31) when use of 100 g of red meat per day, and 18% increase (95% CI of 1.10 to 1.28) by eating 50 g of processed meat per day.
Data were also available in more than 15 other types of cancer. In cohort studies and population research method “case-control” was seen positive correlation between red meat consumption and cancer of the pancreas and prostate (mainly the latter), as well as between culinary consumption of processed meat and stomach cancer.
Based on the large amount of data and consistently obtained correlations of colorectal cancer with consumption of processed meat cooking in various studies of different populations (which makes the accident of obtaining the data, bias and error researchers unlikely because of the presence of evidence), the majority of the members of the working group came to the conclusion that the study of human population there are enough studies of the Carcinogenicity of consumption of processed meat.
Chance, bias and errors cannot be excluded with the same degree of confidence for data on the consumption of red meat, as several studies have high quality was not seen clearly and is also difficult to exclude these impacts, like the rest of the diet and lifestyle. The working group came to the conclusion that there are too few studies of the Carcinogenicity of consumption of red meat in the study of human population.
There is insufficient evidence in experiments on experimental animals for the Carcinogenicity of consumption of red meat and processed. Rats taking carcinogenic drugs and who were on diets with low calcium containing diet of red or processed meat, reported an increase in the incidence of precancerous lesions of the colon in three and four studies, respectively.
Mechanistic evidence of Carcinogenicity was subjected to careful evaluation in the case of the consumption of red meat and was estimated not strictly the consumption of processed meat.
Mechanistic evidence mainly obtained for tumors of the gastrointestinal tract. A meta-analysis, published in 2013, reported weak but statistically significant Association between consumption of red or processed meat and colorectal adenoma (precancerous lesion), and a correlation was observed in all studies.
Moderate consumption of red or processed meat is also associated with evidence-based genotoxicity and oxidative stress.
In the human population, observations showed a small but statistically significant Association with a mutation of the APC gene, or methylation of the promoters identified in 75 (43%) and 41st (23%) of the 185 archival samples of cancer of the colon and rectum, respectively.
The consumption of well cooked red meat enhances the bacterial mutagenicity of human urine. In three studies of samples of patients changes of markers of oxidative stress (urine, feces, or blood) were associated with the consumption of red or processed meat. Also been found to increase the number of products of LPO (lipid peroxidation) in the feces of rodents.
A significant justification of the mechanistic evidence is available for several components of meat (NOC, heme iron, and NAA). The consumption of red and processed cooking meat induces the formation of NOC in the colon.
High consumption of red meat (300 or 420 g/day) increases the level of DNA adducts presumably formed from NOC and found in the exfoliated colonocyte or rectal biopsies in two interventional studies.
For processed meat there are too few available data on the study of its consumption in human populations, especially intervention studies. Heme iron mediates the formation of NOC and LPO products in the digestive tract of man and rodents. In the experiment, the effects of its effects can be suppressed through calcium, supporting its contribution to carcinogenesis.
Meat cooked at high temperatures, contains NAA. This compound is genotoxic, and the degree of conversion of NAA to genotoxic metabolites in humans is higher than in rodents. Smoked and cooked on the heated surface or open flame meat contains PAHs. These chemicals cause DNA damage, however there is little direct evidence that this is the result of eating meat.
60 facts that is useful to know everyone
Nikolai Kozlov: Why I don't eat meat
Insights
In General, the working group classified the consumption of processed meat as "carcinogenic to humans" (risk group 1) based on sufficient evidence of colorectal cancer. In addition, a positive correlation with the culinary consumption of processed meat was found for stomach cancer. The working group has classified the consumption of red meat, as "probably carcinogenic to humans" (group 2A risk).
In conducting this assessment, the panel took into consideration all relevant data, including significant epidemiological data showing a positive Association between the consumption of red meat and colorectal cancer, as well as important mechanistic evidence. The consumption of red meat was also positively associated with pancreatic cancer, and prostate cancer.published
Translation: Dan Raskin
Source: medach.pro/surgery/onkologiya-hirurgicheskie-distsiplinyi/meat-cancer/
Red meat — unprocessed part of the muscles of mammals, such as beef, veal, pork, mutton, lamb, beef or goat meat, including minced meat or frozen meat; commonly used after cooking.
Processed meat — meat, prepared by salting, boiling, fermentation, Smoking or other processes to improve the taste or increase shelf life. Most often, processed meat is pork or beef, but it can also include other varieties, poultry, offal, or offal, such as liver or blood.
Red meat contains proteins of high biological value and important minerals such as b vitamins, iron (free and associated with the heme) and zinc. The fat content of red meat varies according to animal species, age, sex, breeds, feeds and parts of the carcass.
Meat processing, for example, cooking or Smoking, can lead to the formation of carcinogenic chemicals, including N-nitroso-compounds (NOC) and polycyclic aromatic hydrocarbons (PAHs).
Cooking not only improves the digestibility and palatability of meat, but may cause the formation to known or suspected carcinogens, including heterocyclic aromatic amines (haa) and PAHs. Cooking food at high temperatures via frying, grilling or barbecue, in General, produces the greatest number of these compounds.
The average level of consumption of red meat among ordinary consumers is about 50-100 g per person per day, with a high level of consumption is estimated at more than 200 g per person per day.
The consumption of processed meat available information less. The working group assessed more than 800 epidemiological studies examining the correlation of cancer incidence with the consumption of red or processed meat in many countries on several continents, and involving the various ethnic groups and diets.
The most significant for the evaluation was a prospective cohort study conducted in the General population. High-quality sampling study on the basis of the General population provide additional evidence.
In drafting both those, and others, considered to be the most informative studies were those that considered separately the consumption of red and processed meat, had quantitative information on diet is obtained from the verified questionnaire, a large sample size and controlled for the major potential confounders (confounding factors, approx. ed.) relating to the location of the tumor.

The largest array of epidemiological data for colorectal cancer. Data on the correlation of consumption of red meat with colorectal cancer were obtained from 14 cohort studies. A positive correlation was observed at high levels of consumption of red meat (compared to low) in half of these studies, including cohort study based on a sample of residents of ten European countries, covering a wide range of meat consumption, as well as other large cohort studies from Sweden and Australia.
Of the 15 considered informative research method case-control, seven reported a positive correlation of colorectal cancer with high consumption of red meat (compared with lowest consumption level). Positive correlation of this disease with the consumption of processed meat was found in 12 of the 18 cohort studies that provided relevant data, including studies in Europe, Japan and the United States.
Supporting data came from six of the nine informative research method “case-control”. A meta-analysis of ten cohort studies of colorectal cancer reported a statistically significant relationship “dose-response”, with a 17% increased risk (95% CI (confidence interval) of 1.05 to 1.31) when use of 100 g of red meat per day, and 18% increase (95% CI of 1.10 to 1.28) by eating 50 g of processed meat per day.
Data were also available in more than 15 other types of cancer. In cohort studies and population research method “case-control” was seen positive correlation between red meat consumption and cancer of the pancreas and prostate (mainly the latter), as well as between culinary consumption of processed meat and stomach cancer.
Based on the large amount of data and consistently obtained correlations of colorectal cancer with consumption of processed meat cooking in various studies of different populations (which makes the accident of obtaining the data, bias and error researchers unlikely because of the presence of evidence), the majority of the members of the working group came to the conclusion that the study of human population there are enough studies of the Carcinogenicity of consumption of processed meat.
Chance, bias and errors cannot be excluded with the same degree of confidence for data on the consumption of red meat, as several studies have high quality was not seen clearly and is also difficult to exclude these impacts, like the rest of the diet and lifestyle. The working group came to the conclusion that there are too few studies of the Carcinogenicity of consumption of red meat in the study of human population.
There is insufficient evidence in experiments on experimental animals for the Carcinogenicity of consumption of red meat and processed. Rats taking carcinogenic drugs and who were on diets with low calcium containing diet of red or processed meat, reported an increase in the incidence of precancerous lesions of the colon in three and four studies, respectively.
Mechanistic evidence of Carcinogenicity was subjected to careful evaluation in the case of the consumption of red meat and was estimated not strictly the consumption of processed meat.
Mechanistic evidence mainly obtained for tumors of the gastrointestinal tract. A meta-analysis, published in 2013, reported weak but statistically significant Association between consumption of red or processed meat and colorectal adenoma (precancerous lesion), and a correlation was observed in all studies.
Moderate consumption of red or processed meat is also associated with evidence-based genotoxicity and oxidative stress.
In the human population, observations showed a small but statistically significant Association with a mutation of the APC gene, or methylation of the promoters identified in 75 (43%) and 41st (23%) of the 185 archival samples of cancer of the colon and rectum, respectively.
The consumption of well cooked red meat enhances the bacterial mutagenicity of human urine. In three studies of samples of patients changes of markers of oxidative stress (urine, feces, or blood) were associated with the consumption of red or processed meat. Also been found to increase the number of products of LPO (lipid peroxidation) in the feces of rodents.
A significant justification of the mechanistic evidence is available for several components of meat (NOC, heme iron, and NAA). The consumption of red and processed cooking meat induces the formation of NOC in the colon.
High consumption of red meat (300 or 420 g/day) increases the level of DNA adducts presumably formed from NOC and found in the exfoliated colonocyte or rectal biopsies in two interventional studies.
For processed meat there are too few available data on the study of its consumption in human populations, especially intervention studies. Heme iron mediates the formation of NOC and LPO products in the digestive tract of man and rodents. In the experiment, the effects of its effects can be suppressed through calcium, supporting its contribution to carcinogenesis.
Meat cooked at high temperatures, contains NAA. This compound is genotoxic, and the degree of conversion of NAA to genotoxic metabolites in humans is higher than in rodents. Smoked and cooked on the heated surface or open flame meat contains PAHs. These chemicals cause DNA damage, however there is little direct evidence that this is the result of eating meat.
60 facts that is useful to know everyone
Nikolai Kozlov: Why I don't eat meat
Insights
In General, the working group classified the consumption of processed meat as "carcinogenic to humans" (risk group 1) based on sufficient evidence of colorectal cancer. In addition, a positive correlation with the culinary consumption of processed meat was found for stomach cancer. The working group has classified the consumption of red meat, as "probably carcinogenic to humans" (group 2A risk).
In conducting this assessment, the panel took into consideration all relevant data, including significant epidemiological data showing a positive Association between the consumption of red meat and colorectal cancer, as well as important mechanistic evidence. The consumption of red meat was also positively associated with pancreatic cancer, and prostate cancer.published
Translation: Dan Raskin
Source: medach.pro/surgery/onkologiya-hirurgicheskie-distsiplinyi/meat-cancer/