352
Mammography is the reverse side of the coin
From Dr. Mercol.
Mammography is said to reduce your risk of dying from breast cancer by 20 percent, but if you don’t understand where that number comes from, you’re greatly overestimating the potential benefits of a regular mammogram.
In addition, most doctors don’t inform patients about the other side of the process, which is that it actually hurts women more than it helps.

Regular mammograms save 1 in 1,000 women, and 10 women are treated for cancer for no reason.
It may sound incredible, but the 20 percent reduction in mortality risk trumpeted by conventional medicine actually means just 1 in 1,000 women who have regular mammograms. How is that possible?
Of every 1,000 women who do not have a mammogram, 5 die from breast cancer. Of every 1,000 women who have a mammogram, 4 still die.
The difference between the two groups is 20 percent (that one person in the mammogram group who survives). On the other hand, out of every 1,000 women who have regular mammograms over the course of their lives:
Comparing breast cancers diagnosed in women over the age of 40 between 1975 and 1979, before mammography became common, and between 2000 and 2002, three key findings emerged.
At the same time, the sharp increase in the percentage of small tumors is mainly due to overdiagnosis – an estimated 81 percent of these small tumors actually do not require treatment.
The fact that the incidence rate of metastatic cancer remains stable suggests that in most cases we do not detect this species in the early stages. Instead, we identify and treat mostly harmless tumors.
The researchers also found that a two-third reduction in breast cancer mortality was associated with better treatments, such as tamoxifen. Breast cancer screening accounts for only a one-third reduction in mortality.
Examination as a personal choice
In an interview with NBC News, Welch said, “The survey is a choice.” This is not a public health requirement.” Nowadays, most traditional medical oncologists genuinely consider mammograms mandatory, although the recommendations depend on who you listen to.
As of last year, the American Cancer Society (AOE) recommended that women in the middle-risk group have their first mammograms at age 45 and then every year before age 55. Women 55 and older are advised to have a mammogram every two years.
Meanwhile, the U.S. Special Preventive Services Task Force (USPSTF) recommends waiting up to 50 years before getting a mammogram every two years. In response to a heated debate over various recommendations, Congress passed legislation requiring insurance companies to cover the cost of mammograms regardless of age.
Unsurprisingly, the ABO has sharply criticized the latest study. In a statement, the EPA’s chief cancer control officer, Dr. Richard Wender, said: “These presumptuous findings are only intended to attract attention and should be treated with a degree of skepticism – I would say with a fair amount of skepticism.”
The problem with Wender’s attitude is that this is far from the first or only study to suggest that the benefits of mammography are greatly exaggerated. In fact, a number of studies have already disproved the validity of mammography as a major tool in the fight against breast cancer.
Evidence strongly refutes the value of routine mammography
Archives of Internal Medicine, 2007: A meta-analysis of 117 randomized controlled clinical trials of mammography. Among the findings: high rate of false positives: 56 percent after 10 mammograms.
Cochrane Database Review, 2009: This review found 30 percent of cases of overdiagnosis and treatment based on breast cancer screening, which essentially increased the absolute risk of cancer by 0.5 percent.
The review concluded that out of every 2,000 women invited for 10 years, only one woman was able to prolong life, and 10 healthy women received treatment unnecessarily.
New England Bulletin of Medicine, 2010: The study found that the reduction in mortality from mammography screening was so small that it could be considered insignificant, preventing only 2.4 deaths per 100,000 person-years.
Lancet. Oncology 2011: This study describes the natural history of breast cancer identified during the Swedish mammography program between 1986 and 1990, which involved 650,000 women.
Because neoplasms and breast tumors are intensively treated and/or removed before an obvious and real threat to health is established with certainty, very few studies have examined the consequences of discontinuing such treatment.
However, this study showed for the first time that women who underwent the highest number of breast examinations had a higher cumulative incidence of invasive breast cancer over the next six years than the control group, which did much fewer examinations.
The Lancet, 2012:It shows that for every life saved by mammography, there are three cases of overdiagnosis and surgical treatment, radiation or chemotherapy for cancer that may not have bothered them for the rest of their lives.
Cochrane Database Review, 2013: A review of 10 studies involving more than 600,000 women concluded that mammography had no effect on overall mortality.
New England Bulletin of Medicine, 2014: Drs. Nicola Biller-Andorno and Peter Uni published an article in which they described the results of an initiative to independently evaluate health technologies to evaluate the effectiveness of mammography, in which they participated:
First, we noticed that the ongoing discussions are based on a series of reanalyses of the same largely outdated trials. Could the modest, in terms of breast cancer mortality, benefit of mammography found in 1963-1991 studies be confirmed by trials to date?
Second, we were amazed at how unobvious the benefits of mammography outweighed the harms.
Reducing the relative risk of breast cancer mortality by about 20 percent as a result of mammography, which is currently described by most expert groups, came at the cost of a significant diagnostic cascade, with repeated mammography, follow-up biopsies, and overdiagnosis of breast cancer - a cancer that would never clinically manifest. . .
Third, we were confused by the marked discrepancy between the real benefits of mammography and how women imagine them.
British Medical Journal, 2014: According to the results of the Canadian study, the rate of overdiagnosis and overtreatment on the results of mammography was almost 22 percent.
Herald of Internal Medicine, andJuly 2015: Here, researchers concluded that mammography results in unnecessary treatment and has virtually no effect on the number of breast cancer deaths. A positive correlation between breast cancer screening and breast cancer incidence was indeed established, but no positive correlation with mortality was found.
Bulletin of the Royal Medical Society, September 2015: The conclusion of this study is already stated in the title itself, which reads: “Mammographic examination is harmful and should be abandoned.”
In short, the authors concluded that decades of routine mammography screening did not reduce breast cancer mortality, but that more than half (52 percent) of all women screened were overdiagnosed and unnecessarily treated.

Data on vitamin D as a means of preventing cancer
Mammography is portrayed as the best kind of “prevention” a woman can get. Early diagnosis is not the same as prevention. And if cancer screening does more harm than good, how can you call it the best option? I think when it comes to mammography, the evidence speaks for itself.
The same can be said for vitamin D studies, which repeatedly show that optimizing vitamin D levels to 40-60 nanograms per milliliter (ng/ml) provides serious protection against cancer. I believe that a blood test for vitamin D levels is one of the most important tests for cancer prevention. Ideally, it should be taken twice a year.
Of course, there are exceptions. If you feel a lump in your chest, mammography may be warranted, although even then there are other non-ionizing options, such as ultrasound, which has been shown to be significantly superior to mammography, especially for women with dense breasts who are at increased risk of false negative mammography results.
One of the most recent studies examining vitamin D in breast cancer found that vitamin D deficiency is associated with tumor growth and metastasis. As Stanford University researcher Dr. Brian Feldman notes:
A number of large studies have looked for a link between vitamin D levels and cancer outcomes, and the results have been mixed. Our study identifies how low levels of vitamin D circulating in the blood may play a mechanistic role in promoting breast cancer growth and metastasis.
Higher levels of vitamin D have also been linked to an increased likelihood of survival after a breast cancer diagnosis. In one study, patients with breast cancer and blood levels of vitamin D had an average death rate of 30 ng/ml 50 percent lower than those with an average of 17 ng/ml.
I am very grateful that the medical community has taken vitamin D into consideration and started using it. However, it’s important to understand that the best way to get vitamin D is to stay in the sun for a reasonable time, and if you’re really interested in optimal health and healing, you’ll do everything in your power to achieve that. That's one of the reasons I moved to Florida. I haven’t swallowed a single vitamin D pill in 8 years, but my blood levels are over 60 ng/ml.
There are many other benefits of sun exposure besides vitamin D. More than 40 percent of sunlight is near-infrared, which the body needs to structure water and stimulate mitochondrial repair and regeneration. If you only ingest vitamin D and avoid the sun, you deprive yourself of the main benefit of reasonable sun exposure.
Glycation and its products: Garbage inside your body Teeth hurt in hesitant people or what the problems with the teeth say
If it’s eternal winter and you’re low in vitamin D, it might be better to take oral vitamin D supplements as medicine, but remember that this is a WORST way to optimize your vitamin D levels, and by avoiding exposure to sunlight, you’re missing out on many important biological benefits.
Source: russian.mercola.com/sites/articles/archive/2016/11/22/%D0%BC%D0%B0%D0%BC%D0%B0%BE%D0%B0%B3%D1%80%D0%B0%D1%84%D0%B8%D1%8F-%D1%8D1%8D1%8D1%84%D0%B5%D0%D1%82%D1%8B-%D1%8D1%8D1%D1%8D0%D0%B-%D1%8D0%D0%D0%B%D0%B8D0%D0%D0%B%D0%B8D0%D0%D0%B%D0%B%D0%B8D0%B%D0%B8D0%D0%D0%D0%B%D0%B%D0%B8D0%D0%B%D0%B8D0%B%D0%B8D0%D0%B%D0%B8D0%D0%D0%D0%B%D0%B%D0%B8D%D0%B8D0%B%D%D0%B%D0%
Mammography is said to reduce your risk of dying from breast cancer by 20 percent, but if you don’t understand where that number comes from, you’re greatly overestimating the potential benefits of a regular mammogram.
In addition, most doctors don’t inform patients about the other side of the process, which is that it actually hurts women more than it helps.

Regular mammograms save 1 in 1,000 women, and 10 women are treated for cancer for no reason.
It may sound incredible, but the 20 percent reduction in mortality risk trumpeted by conventional medicine actually means just 1 in 1,000 women who have regular mammograms. How is that possible?
Of every 1,000 women who do not have a mammogram, 5 die from breast cancer. Of every 1,000 women who have a mammogram, 4 still die.
The difference between the two groups is 20 percent (that one person in the mammogram group who survives). On the other hand, out of every 1,000 women who have regular mammograms over the course of their lives:
- Half will get a false positive. That is, they will NOT have cancer, but about 500 out of every 1,000 women who have a mammogram will face the horror of being diagnosed with breast cancer.
- 64 will do a biopsy - a painful procedure associated with the risk of adverse consequences
- 10 will receive treatment for cancer (although they will NOT have cancer), including disfiguring operations, taking toxic drugs, or receiving radiation therapy. Surgery, chemotherapy and radiation therapy are all risky, but dying from treatment for non-existent cancer is doubly tragic.
Comparing breast cancers diagnosed in women over the age of 40 between 1975 and 1979, before mammography became common, and between 2000 and 2002, three key findings emerged.
- The percentage of patients with large tumors (2 centimeters or more) decreased from 68 percent to 32 percent.
- The percentage of women diagnosed with small tumors increased from 36 to 64 percent
- Percentage of patients with metastatic cancer, which is the deadliest, unchanged
At the same time, the sharp increase in the percentage of small tumors is mainly due to overdiagnosis – an estimated 81 percent of these small tumors actually do not require treatment.
The fact that the incidence rate of metastatic cancer remains stable suggests that in most cases we do not detect this species in the early stages. Instead, we identify and treat mostly harmless tumors.
The researchers also found that a two-third reduction in breast cancer mortality was associated with better treatments, such as tamoxifen. Breast cancer screening accounts for only a one-third reduction in mortality.
Examination as a personal choice
In an interview with NBC News, Welch said, “The survey is a choice.” This is not a public health requirement.” Nowadays, most traditional medical oncologists genuinely consider mammograms mandatory, although the recommendations depend on who you listen to.
As of last year, the American Cancer Society (AOE) recommended that women in the middle-risk group have their first mammograms at age 45 and then every year before age 55. Women 55 and older are advised to have a mammogram every two years.
Meanwhile, the U.S. Special Preventive Services Task Force (USPSTF) recommends waiting up to 50 years before getting a mammogram every two years. In response to a heated debate over various recommendations, Congress passed legislation requiring insurance companies to cover the cost of mammograms regardless of age.
Unsurprisingly, the ABO has sharply criticized the latest study. In a statement, the EPA’s chief cancer control officer, Dr. Richard Wender, said: “These presumptuous findings are only intended to attract attention and should be treated with a degree of skepticism – I would say with a fair amount of skepticism.”
The problem with Wender’s attitude is that this is far from the first or only study to suggest that the benefits of mammography are greatly exaggerated. In fact, a number of studies have already disproved the validity of mammography as a major tool in the fight against breast cancer.
Evidence strongly refutes the value of routine mammography
Archives of Internal Medicine, 2007: A meta-analysis of 117 randomized controlled clinical trials of mammography. Among the findings: high rate of false positives: 56 percent after 10 mammograms.
Cochrane Database Review, 2009: This review found 30 percent of cases of overdiagnosis and treatment based on breast cancer screening, which essentially increased the absolute risk of cancer by 0.5 percent.
The review concluded that out of every 2,000 women invited for 10 years, only one woman was able to prolong life, and 10 healthy women received treatment unnecessarily.
New England Bulletin of Medicine, 2010: The study found that the reduction in mortality from mammography screening was so small that it could be considered insignificant, preventing only 2.4 deaths per 100,000 person-years.
Lancet. Oncology 2011: This study describes the natural history of breast cancer identified during the Swedish mammography program between 1986 and 1990, which involved 650,000 women.
Because neoplasms and breast tumors are intensively treated and/or removed before an obvious and real threat to health is established with certainty, very few studies have examined the consequences of discontinuing such treatment.
However, this study showed for the first time that women who underwent the highest number of breast examinations had a higher cumulative incidence of invasive breast cancer over the next six years than the control group, which did much fewer examinations.
The Lancet, 2012:It shows that for every life saved by mammography, there are three cases of overdiagnosis and surgical treatment, radiation or chemotherapy for cancer that may not have bothered them for the rest of their lives.
Cochrane Database Review, 2013: A review of 10 studies involving more than 600,000 women concluded that mammography had no effect on overall mortality.
New England Bulletin of Medicine, 2014: Drs. Nicola Biller-Andorno and Peter Uni published an article in which they described the results of an initiative to independently evaluate health technologies to evaluate the effectiveness of mammography, in which they participated:
First, we noticed that the ongoing discussions are based on a series of reanalyses of the same largely outdated trials. Could the modest, in terms of breast cancer mortality, benefit of mammography found in 1963-1991 studies be confirmed by trials to date?
Second, we were amazed at how unobvious the benefits of mammography outweighed the harms.
Reducing the relative risk of breast cancer mortality by about 20 percent as a result of mammography, which is currently described by most expert groups, came at the cost of a significant diagnostic cascade, with repeated mammography, follow-up biopsies, and overdiagnosis of breast cancer - a cancer that would never clinically manifest. . .
Third, we were confused by the marked discrepancy between the real benefits of mammography and how women imagine them.
British Medical Journal, 2014: According to the results of the Canadian study, the rate of overdiagnosis and overtreatment on the results of mammography was almost 22 percent.
Herald of Internal Medicine, andJuly 2015: Here, researchers concluded that mammography results in unnecessary treatment and has virtually no effect on the number of breast cancer deaths. A positive correlation between breast cancer screening and breast cancer incidence was indeed established, but no positive correlation with mortality was found.
Bulletin of the Royal Medical Society, September 2015: The conclusion of this study is already stated in the title itself, which reads: “Mammographic examination is harmful and should be abandoned.”
In short, the authors concluded that decades of routine mammography screening did not reduce breast cancer mortality, but that more than half (52 percent) of all women screened were overdiagnosed and unnecessarily treated.

Data on vitamin D as a means of preventing cancer
Mammography is portrayed as the best kind of “prevention” a woman can get. Early diagnosis is not the same as prevention. And if cancer screening does more harm than good, how can you call it the best option? I think when it comes to mammography, the evidence speaks for itself.
The same can be said for vitamin D studies, which repeatedly show that optimizing vitamin D levels to 40-60 nanograms per milliliter (ng/ml) provides serious protection against cancer. I believe that a blood test for vitamin D levels is one of the most important tests for cancer prevention. Ideally, it should be taken twice a year.
Of course, there are exceptions. If you feel a lump in your chest, mammography may be warranted, although even then there are other non-ionizing options, such as ultrasound, which has been shown to be significantly superior to mammography, especially for women with dense breasts who are at increased risk of false negative mammography results.
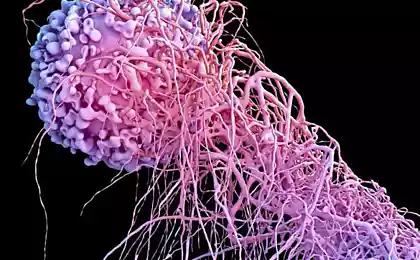
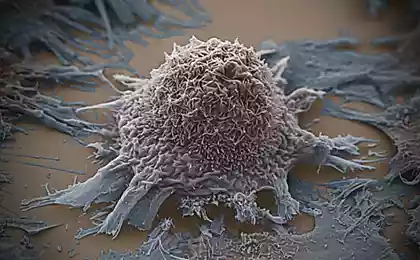
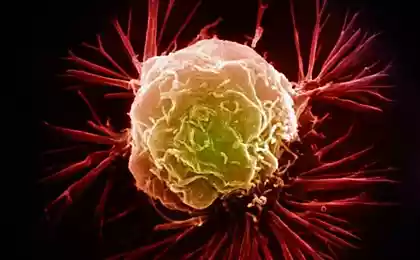
One of the most recent studies examining vitamin D in breast cancer found that vitamin D deficiency is associated with tumor growth and metastasis. As Stanford University researcher Dr. Brian Feldman notes:
A number of large studies have looked for a link between vitamin D levels and cancer outcomes, and the results have been mixed. Our study identifies how low levels of vitamin D circulating in the blood may play a mechanistic role in promoting breast cancer growth and metastasis.
Higher levels of vitamin D have also been linked to an increased likelihood of survival after a breast cancer diagnosis. In one study, patients with breast cancer and blood levels of vitamin D had an average death rate of 30 ng/ml 50 percent lower than those with an average of 17 ng/ml.
I am very grateful that the medical community has taken vitamin D into consideration and started using it. However, it’s important to understand that the best way to get vitamin D is to stay in the sun for a reasonable time, and if you’re really interested in optimal health and healing, you’ll do everything in your power to achieve that. That's one of the reasons I moved to Florida. I haven’t swallowed a single vitamin D pill in 8 years, but my blood levels are over 60 ng/ml.
There are many other benefits of sun exposure besides vitamin D. More than 40 percent of sunlight is near-infrared, which the body needs to structure water and stimulate mitochondrial repair and regeneration. If you only ingest vitamin D and avoid the sun, you deprive yourself of the main benefit of reasonable sun exposure.
Glycation and its products: Garbage inside your body Teeth hurt in hesitant people or what the problems with the teeth say
If it’s eternal winter and you’re low in vitamin D, it might be better to take oral vitamin D supplements as medicine, but remember that this is a WORST way to optimize your vitamin D levels, and by avoiding exposure to sunlight, you’re missing out on many important biological benefits.
Source: russian.mercola.com/sites/articles/archive/2016/11/22/%D0%BC%D0%B0%D0%BC%D0%B0%BE%D0%B0%B3%D1%80%D0%B0%D1%84%D0%B8%D1%8F-%D1%8D1%8D1%8D1%84%D0%B5%D0%D1%82%D1%8B-%D1%8D1%8D1%D1%8D0%D0%B-%D1%8D0%D0%D0%B%D0%B8D0%D0%D0%B%D0%B8D0%D0%D0%B%D0%B%D0%B8D0%B%D0%B8D0%D0%D0%D0%B%D0%B%D0%B8D0%D0%B%D0%B8D0%B%D0%B8D0%D0%B%D0%B8D0%D0%D0%D0%B%D0%B%D0%B8D%D0%B8D0%B%D%D0%B%D0%
Where are the black stripes in life after white
This drink will make your hair and skin healthy and glowing