555
Metabolic memory: revenge served cold
Glycation (glycation) leads not only to structural but also functional changes in many elements of the body. Moreover, these changes are long-term, from several months to several years (6 years or more). This phenomenon was named "metabolic memory", today I will explain how glycation may rebuild a normal cell exchange and why the lifestyle change may not always work effectively immediately.
Dorogobush glycation of proteins and DNA is a process that is imperceptible at first, but then very trudnosravnimyh. Yes, the final products of glycosylation can be very vindictive and revenge is a dish best served cold.
Twenty two million eight hundred sixteen thousand nine hundred twenty four
What is the metabolic memory?
The term "metabolic memory" appeared in the study of diabetes. The fact is that, despite advances in the treatment of diseases – the development of new antidiabetic means, the achievement of successful glycemic control and identification of markers of blood glucose levels, most patients develop severe damage to target organs, leading to serious complications.
Metabolic memory (less known as or vascular hyperglycemic memory) is the effect, leading to the development of long-term consequences of a long period of poorly compensated glucose level of blood. In other words, the longer diabetes remains uncompensated, the longer persists this destructive effect, even after improving the control of the disease.
Elementary, early episodes of hyperglycemia have a negative impact on the level of cells in the retina, kidneys, and the functioning of the nerve fibers. "Metabolic memory" is a situation when the increase of glycaemia before diagnosis of the disease is already pathologically affects multiple systems of the body in the first place, nerve fibers. Furthermore, if glycemic control has long been insufficient, damage may continue in the future, even after optimization of glucose level.
In particular, extensive research in ADVANCE revealed that strict control of glycemia in diabetes mellitus (DM) type 2 have only led to a reduction in the incidence of nephropathy, with the incidence of retinopathy and macrovascular complications not reduced. The results of another large-scale study of the ACCORD demonstrated that strict glycemic control has led to an increase in mortality among patients with type 2 diabetes.
In the UKPDS study did not identify any significant implications of tight glycemic control on myocardial infarction. Promising direction is the approach based on the assumption that hyperglycemia exerts long-term adverse effects in diabetes mellitus 1 and 2 types and strict glycemic control, if it is not provided in the very early stages of the disease, is not sufficient to fully prevent complications.
Seventy six million five hundred seventy three thousand six hundred sixty five
The basis of this hypothesis lies the idea of the phenomenon of metabolic memory which is that early glycemic background "remembered" in the tissues and target organs (retina, kidney, heart, peripheral nerves). The first data confirmed the existence of metabolic memory have been obtained in animal experiments in the study of retinal cells of dogs, one group of which were translated into a strict control of glycemia after two months and the other after 2.5 years of hyperglycemia.
The study of the retina was carried out 5 years after the start of the experiment. Paradoxically, in animals, in which the control of glycemia started 2 months, there were slight signs of retinopathy, as well as in animals with glycemic control throughout the study period. At the same time in dogs, which have been translated into strict glycemic control in 2.5 years, the frequency of retinopathy was similar to the level of retinopathy in dogs that were in a state of hyperglycemia for 5 years.
The term "metabolic memory" has several synonyms – glycemic memory hyperglycemic memory and hereditary effects and other. Clinical confirmation of the phenomenon of metabolic memory was obtained during a large-scale clinical studies type 1 diabetes DCCT (Diabetes Complications and Control Trial) and follow-up study EDIC (Epidemiology of Diabetes Interventions and Complications). During the DCCT patients with diabetes type 1 were divided into 2 groups – insulinoterapii intensified and conventional therapy aimed at normalization of glycemia.
Later in the study, EDIC, conducted on the same population of patients, it was found that the participants who underwent the standard therapy during the DCCT, the incidence of microvascular complications such as nephropathy and retinopathy was higher compared with patients intensified therapy, although after 6.5 years, all study participants were transferred to intensified therapy.
Another interesting fact – in both groups the average level of glycated hemoglobin was almost equivalent. In addition, the recent EDIC results confirm the long-term effect of early glycemic control on the progression of macrovascular complications and cardiovascular diseases.
The phenomenon of metabolic memory has also been identified with diabetes type 2 the results of the study UKPDS (U.K. Prospective Diabetes Study). In patients with type 2 diabetes who were on standard therapy during the study, the level of microvascular and cardiovascular complications was higher compared with patients who received intensive therapy.
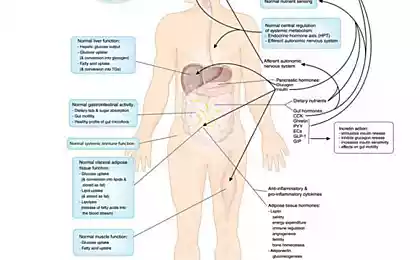
The damaging effect of hyperglycemia on the cellular level is implemented using four well-known mechanisms: induction Paleologo way implemented through aldozoredouktazu enzyme; increased formation of end products excessive glycosylation (AGE); activation of protein kinase C; activation hexosaminidase way.
The significance of each of these mechanisms has been repeatedly confirmed in animal studies using different inhibitors of a particular path of biochemical reactions, thus preventing diabetic complications. However, the problem was that, despite the obvious success of the use of inhibitors in animal experiments, using the same preparations in the treatment of patients the results were extremely unsatisfactory.
In further studies, it was found that all four of the pathological reactions triggered in response to the increased production of superoxide anion in the respiratory chain of mitochondria, a process induced by hyperglycemia. The formation of superoxide occurs under the influence of high intracellular concentrations of glucose, disrupting the components of the respiratory chain of mitochondria and transfers electrons to the oxygen molecule.
If the generation of a large amount of superoxide anion is a key process in the development of diabetic complications, how important a role it plays in the phenomenon of metabolic memory? Superoxide, like most reactive molecules (radicals), has a very short half – life not longer than a minute, whereas glycemic memory can last for years.
In fact, targets for the superoxide ions and other radicals serve as nucleic acids, proteins, lipids and lipoproteins with long half-life. These molecules are damaged by radicals that may damage the operation of cells for a long time.
Connection 3-nitrogen, the product of the interaction of free radicals with cellular proteins, can serve as an important marker of oxidative stress in the complications of diabetes. This substance has been used in numerous experiments in animal models, which demonstrated the role of oxidative stress in the formation of the glycemic memory.
For example, R. A. Kowluru et al. found that in rats with streptozotocin-induced diabetes, normalization of blood glucose levels within 6 months after the 6-month period of hyperglycemia does not lead to a significant decrease in the level of 3-nitrozine in the retinal cells, as well as in animals in which hyperglycemia was maintained throughout the study. Once again I draw your attention – for six months, nothing has changed, and it had rats!
АGE-Produkty is a metabolic substrate of memory.
Along with oxidative stress the mitochondria of cells subjected to other adverse effects of hyperglycemia – glycation of mitochondrial proteins. In particular, it was found that the level of methylglyoxal is highly reactive by-product of glycolysis – is elevated in patients with diabetes.
Methylglyoxal reacts with proteins and nucleic acids of the cell, forms the so-called final products of excessive glycation – advanced glycation end-products (AGE). AGE-products play a key role in the development of diabetic complications.
Glycation of proteins of the respiratory chain of mitochondria leading to disruption of its work and maintaining the formation of excess superoxide ions regardless of the level of glycemia. In addition, the formation of AGE-products in the structure of mitochondria, being an irreversible process, may also explain the continued existence of the metabolic memory.
Thirty four million thirty thousand three hundred eighty four
It is shown that in diabetic patients the level of AGE products in tissues elevated compared with healthy people. Moreover, the patients with diabetes without complications, the level of AGE products increased by 20-30%, and diabetes in combination with cardiovascular complications or microalbuminuria – by 40-100% compared with healthy people.
During the EDIC study, the levels of AGE products, determined by skin biopsy, significantly correlated with the prevalence of retinopathy and nephropathy. Unlike glycated hemoglobin, which by reducing blood glucose undergoes partial enzymatic deglycosylation, the level of other AGE-products depends on the current glucose level.
In addition to the direct participation of AGE-products in the formation of metabolic memory play the role of their receptors, in particular the type of receptor, called RAGE, which belongs to the immunoglobulin superfamily of cell surface molecules.
AGE and binding of this receptor leads to the formation of reactive oxygen species (ROS) with subsequent activation of oxidation-sensitive transcription factor NF-KB in the vascular wall, regulating the expression of inflammatory and "responding to damage" genes and directly gene RAGE.
These events ultimately lead to endothelial dysfunction and, as a consequence, vasoconstriction, inflammatory phenomena, thickening of the basal membrane and decreased ability to vasodilation. The negative effects of AGE-products are sold not only in the walls of vessels, but also in neurons and even in the bone. In the neurons of AGE-products provoke the gradual destruction of nerve fibers. Glycation of proteins of the respiratory chain of mitochondria together with damage to mitochondrial DNA can lead to the formation of new generations of the AFC, persistent oxidative stress and cellular damage.
Seventy six million nine hundred ninety four thousand one hundred forty nine
Vicious circle: АGE-RAGE-inflammation-stress.
This self-sustaining process is the basis of metabolic memory – the leading mechanism of the pathogenesis of diabetic complications, which does not depend on the current level of glycemia. In this context, very promising in terms of prevention of complications are presented the methods "turn off" the metabolic memory.
Previously great hopes were pinned on the use of antioxidants as a key role in the mechanism of injury plays an oxidative stress, but clinical use of these drugs in diabetes have not led to significant improvements. However, it is assumed that the suppression of the formation of AGE-products, the expression of RAGE and oxidative stress in combination with the normalization of blood glucose levels effectively to prevent complications.
Fifty nine million one hundred thirty six thousand nine hundred twenty seven
AGE can also impair cell functions, linking different receptors, including macrophages, endothelial cells and smooth muscle cells in the tissues of the kidneys, and nerve cells. These receptors, interacting with the end products of glycation are called RAGE receptors. RAGE receptors are key mediators in the response of the body to bacteria and viruses.
AGE, glikozilirovanie proteins, lipids and even nucleic acids can act as ligands interacting with RAGE receptor and initiating intracellular signals, including activation of NF-kB, the main inflammatory agent that promotes aging.
Instead join directly to proteins of the type collagen or elastin, these instant AGE act as ligands for RAGE-receptors and provoke an inflammatory process. RAGE-receptors support cell in an enabled state, causing short-term anti-inflammatory response becomes a long cellular dysfunction.
АGE-Poduct and the receptor (RAGE): from vessels to Alzheimer's.
Receptor glycosylation end products (RAGE) is multiligand transmembrane glycoprotein type I, belonging to the superfamily of immunoglobulin (Ig). RAGE may participate in several pathological processes including diabetes, Alzheimer's disease (AD), systemic amyloidosis, and tumor growth.
RAGE was originally characterized based on its ability to bind AGEs, adducts formed by non-enzymatic glycosylation and oxidation of proteins and lipids. This process occurs in normal aging process and dramatically accelerated in diabetes, where hyperglycemia is the main trigger. Substantial evidence support a role for interaction of AGE/RAGE in the pathophysiology of diabetes. Both AGEs and RAGE are elevated in diabetes in the blood vessels, monocytes and podocytes.
RAGE may also mediate physiological functions such as neuronal growth, survival and regeneration, and plays an important role in proinflammatory reactions. RAGE is expressed at a high level in the development process, especially in the Central nervous system (CNS). It is also expressed at a lower level in adult cells: endothelial cells, including smooth muscle cells, mononuclear phagocytes, pericytes, neurons, cardiomyocytes, and hepatocytes. RAGE ligands include the end products of glycation (AGEs), protein amyloid-β (Aß), HMG-1 (also known as amphoteric) and several members of superselective protein S100.
Blockade of RAGE activation of recombinant sRAGE or blocking the function of antibodies reduces vascular permeability, the development of atherosclerotic lesions and enhances wound healing in patients with diabetes mellitus rodents. RAGE-null mice with diabetes do not develop signs of nephropathy, including increased expansion of mesangial matrix and thickening of glomerular membrane.
In contrast, transgenic overexpression of RAGE leads to the aggravation of diabetic nephropathy and retinopathy. RAGE is also a receptor for β-pleated fibrils, structures that are characteristic of amyloid. Aß is the main component of neurodegenerative plaques associated with Alzheimer's disease (AD) and RAGE colocalized with Aß in the brain of patients with asthma at increased amounts.
Sixty five million one hundred fifty five thousand one hundred seventy two
From a molecular point of view, Alzheimer's disease is characterized by deposits of abnormally aggregated proteins. In the case of extracellular amyloid plaques, these deposits mainly consist of filaments of β-amyloid peptides (Aß), in the case of the intracellular neurofibrillary tangles (NFT), mainly of protein tau.
AD is also characterized by increased expression of RAGE in neurons. RAGE is a receptor of the immunoglobulin family that has many ligands, which functions as the transmitting signal of the acceptor Aß on the cell surface. Receptor glycosylation end products (RAGE), which localized not only to neurons, astroglia and microglia, but also on endothelial cells, where it acts as a Transporter of beta-amyloid in the brain from the bloodstream.
Several groups shown that infusion of Aβ40 in mice leads to vasoconstriction of cerebral vessels and weakening of cerebral circulation (CBF). Patients with AD also have poor cerebral circulation. In AD mouse models in which transgenic animals sverkhekspressiya amyloid precursor protein (APP), which leads to disease causing plaque formation, it is demonstrated that RAGE is implicated as a pathogenic factor in the progression of the disease.
It is shown that RAGE binds to Aß-peptides. Inhibition of this interaction suppresses accumulation of Aß in transgenic animal models; therefore, I believe that RAGE is implicated in AD. It is shown that the treatment with sRAGE (soluble RAGE), and anti-RAGE-antibody reduces the number of plaques (Deane et al, 2003). Blocking the interaction of RAGE with amyloid with antibodies can be a suitable method for the treatment of patients with AD; however, the existing polyclonal antibodies obtained from the serum of animals, are not suitable for chronic treatment of humans.published
Author: Andrey Blueskin
See also:
Antiparasitic cleansing and priming
You can treat the nervous system, and hypertension and get a stroke because of ostechondrosis!
P. S. And remember, only by changing their consumption — together we change the world! ©
Join us in Facebook , Vkontakte, Odnoklassniki
Source: www.beloveshkin.com/2016/05/glikirovanie-i-metabolicheskaya-pamyat-mest-podaetsya-kholodnoj.html
Dorogobush glycation of proteins and DNA is a process that is imperceptible at first, but then very trudnosravnimyh. Yes, the final products of glycosylation can be very vindictive and revenge is a dish best served cold.
Twenty two million eight hundred sixteen thousand nine hundred twenty four
What is the metabolic memory?
The term "metabolic memory" appeared in the study of diabetes. The fact is that, despite advances in the treatment of diseases – the development of new antidiabetic means, the achievement of successful glycemic control and identification of markers of blood glucose levels, most patients develop severe damage to target organs, leading to serious complications.
Metabolic memory (less known as or vascular hyperglycemic memory) is the effect, leading to the development of long-term consequences of a long period of poorly compensated glucose level of blood. In other words, the longer diabetes remains uncompensated, the longer persists this destructive effect, even after improving the control of the disease.
Elementary, early episodes of hyperglycemia have a negative impact on the level of cells in the retina, kidneys, and the functioning of the nerve fibers. "Metabolic memory" is a situation when the increase of glycaemia before diagnosis of the disease is already pathologically affects multiple systems of the body in the first place, nerve fibers. Furthermore, if glycemic control has long been insufficient, damage may continue in the future, even after optimization of glucose level.
In particular, extensive research in ADVANCE revealed that strict control of glycemia in diabetes mellitus (DM) type 2 have only led to a reduction in the incidence of nephropathy, with the incidence of retinopathy and macrovascular complications not reduced. The results of another large-scale study of the ACCORD demonstrated that strict glycemic control has led to an increase in mortality among patients with type 2 diabetes.
In the UKPDS study did not identify any significant implications of tight glycemic control on myocardial infarction. Promising direction is the approach based on the assumption that hyperglycemia exerts long-term adverse effects in diabetes mellitus 1 and 2 types and strict glycemic control, if it is not provided in the very early stages of the disease, is not sufficient to fully prevent complications.
Seventy six million five hundred seventy three thousand six hundred sixty five
The basis of this hypothesis lies the idea of the phenomenon of metabolic memory which is that early glycemic background "remembered" in the tissues and target organs (retina, kidney, heart, peripheral nerves). The first data confirmed the existence of metabolic memory have been obtained in animal experiments in the study of retinal cells of dogs, one group of which were translated into a strict control of glycemia after two months and the other after 2.5 years of hyperglycemia.
The study of the retina was carried out 5 years after the start of the experiment. Paradoxically, in animals, in which the control of glycemia started 2 months, there were slight signs of retinopathy, as well as in animals with glycemic control throughout the study period. At the same time in dogs, which have been translated into strict glycemic control in 2.5 years, the frequency of retinopathy was similar to the level of retinopathy in dogs that were in a state of hyperglycemia for 5 years.
The term "metabolic memory" has several synonyms – glycemic memory hyperglycemic memory and hereditary effects and other. Clinical confirmation of the phenomenon of metabolic memory was obtained during a large-scale clinical studies type 1 diabetes DCCT (Diabetes Complications and Control Trial) and follow-up study EDIC (Epidemiology of Diabetes Interventions and Complications). During the DCCT patients with diabetes type 1 were divided into 2 groups – insulinoterapii intensified and conventional therapy aimed at normalization of glycemia.
Later in the study, EDIC, conducted on the same population of patients, it was found that the participants who underwent the standard therapy during the DCCT, the incidence of microvascular complications such as nephropathy and retinopathy was higher compared with patients intensified therapy, although after 6.5 years, all study participants were transferred to intensified therapy.
Another interesting fact – in both groups the average level of glycated hemoglobin was almost equivalent. In addition, the recent EDIC results confirm the long-term effect of early glycemic control on the progression of macrovascular complications and cardiovascular diseases.
The phenomenon of metabolic memory has also been identified with diabetes type 2 the results of the study UKPDS (U.K. Prospective Diabetes Study). In patients with type 2 diabetes who were on standard therapy during the study, the level of microvascular and cardiovascular complications was higher compared with patients who received intensive therapy.
The damaging effect of hyperglycemia on the cellular level is implemented using four well-known mechanisms: induction Paleologo way implemented through aldozoredouktazu enzyme; increased formation of end products excessive glycosylation (AGE); activation of protein kinase C; activation hexosaminidase way.
The significance of each of these mechanisms has been repeatedly confirmed in animal studies using different inhibitors of a particular path of biochemical reactions, thus preventing diabetic complications. However, the problem was that, despite the obvious success of the use of inhibitors in animal experiments, using the same preparations in the treatment of patients the results were extremely unsatisfactory.
In further studies, it was found that all four of the pathological reactions triggered in response to the increased production of superoxide anion in the respiratory chain of mitochondria, a process induced by hyperglycemia. The formation of superoxide occurs under the influence of high intracellular concentrations of glucose, disrupting the components of the respiratory chain of mitochondria and transfers electrons to the oxygen molecule.
If the generation of a large amount of superoxide anion is a key process in the development of diabetic complications, how important a role it plays in the phenomenon of metabolic memory? Superoxide, like most reactive molecules (radicals), has a very short half – life not longer than a minute, whereas glycemic memory can last for years.
In fact, targets for the superoxide ions and other radicals serve as nucleic acids, proteins, lipids and lipoproteins with long half-life. These molecules are damaged by radicals that may damage the operation of cells for a long time.
Connection 3-nitrogen, the product of the interaction of free radicals with cellular proteins, can serve as an important marker of oxidative stress in the complications of diabetes. This substance has been used in numerous experiments in animal models, which demonstrated the role of oxidative stress in the formation of the glycemic memory.
For example, R. A. Kowluru et al. found that in rats with streptozotocin-induced diabetes, normalization of blood glucose levels within 6 months after the 6-month period of hyperglycemia does not lead to a significant decrease in the level of 3-nitrozine in the retinal cells, as well as in animals in which hyperglycemia was maintained throughout the study. Once again I draw your attention – for six months, nothing has changed, and it had rats!
АGE-Produkty is a metabolic substrate of memory.
Along with oxidative stress the mitochondria of cells subjected to other adverse effects of hyperglycemia – glycation of mitochondrial proteins. In particular, it was found that the level of methylglyoxal is highly reactive by-product of glycolysis – is elevated in patients with diabetes.
Methylglyoxal reacts with proteins and nucleic acids of the cell, forms the so-called final products of excessive glycation – advanced glycation end-products (AGE). AGE-products play a key role in the development of diabetic complications.
Glycation of proteins of the respiratory chain of mitochondria leading to disruption of its work and maintaining the formation of excess superoxide ions regardless of the level of glycemia. In addition, the formation of AGE-products in the structure of mitochondria, being an irreversible process, may also explain the continued existence of the metabolic memory.
Thirty four million thirty thousand three hundred eighty four
It is shown that in diabetic patients the level of AGE products in tissues elevated compared with healthy people. Moreover, the patients with diabetes without complications, the level of AGE products increased by 20-30%, and diabetes in combination with cardiovascular complications or microalbuminuria – by 40-100% compared with healthy people.
During the EDIC study, the levels of AGE products, determined by skin biopsy, significantly correlated with the prevalence of retinopathy and nephropathy. Unlike glycated hemoglobin, which by reducing blood glucose undergoes partial enzymatic deglycosylation, the level of other AGE-products depends on the current glucose level.
In addition to the direct participation of AGE-products in the formation of metabolic memory play the role of their receptors, in particular the type of receptor, called RAGE, which belongs to the immunoglobulin superfamily of cell surface molecules.
AGE and binding of this receptor leads to the formation of reactive oxygen species (ROS) with subsequent activation of oxidation-sensitive transcription factor NF-KB in the vascular wall, regulating the expression of inflammatory and "responding to damage" genes and directly gene RAGE.
These events ultimately lead to endothelial dysfunction and, as a consequence, vasoconstriction, inflammatory phenomena, thickening of the basal membrane and decreased ability to vasodilation. The negative effects of AGE-products are sold not only in the walls of vessels, but also in neurons and even in the bone. In the neurons of AGE-products provoke the gradual destruction of nerve fibers. Glycation of proteins of the respiratory chain of mitochondria together with damage to mitochondrial DNA can lead to the formation of new generations of the AFC, persistent oxidative stress and cellular damage.
Seventy six million nine hundred ninety four thousand one hundred forty nine
Vicious circle: АGE-RAGE-inflammation-stress.
This self-sustaining process is the basis of metabolic memory – the leading mechanism of the pathogenesis of diabetic complications, which does not depend on the current level of glycemia. In this context, very promising in terms of prevention of complications are presented the methods "turn off" the metabolic memory.
Previously great hopes were pinned on the use of antioxidants as a key role in the mechanism of injury plays an oxidative stress, but clinical use of these drugs in diabetes have not led to significant improvements. However, it is assumed that the suppression of the formation of AGE-products, the expression of RAGE and oxidative stress in combination with the normalization of blood glucose levels effectively to prevent complications.
Fifty nine million one hundred thirty six thousand nine hundred twenty seven
AGE can also impair cell functions, linking different receptors, including macrophages, endothelial cells and smooth muscle cells in the tissues of the kidneys, and nerve cells. These receptors, interacting with the end products of glycation are called RAGE receptors. RAGE receptors are key mediators in the response of the body to bacteria and viruses.
AGE, glikozilirovanie proteins, lipids and even nucleic acids can act as ligands interacting with RAGE receptor and initiating intracellular signals, including activation of NF-kB, the main inflammatory agent that promotes aging.
Instead join directly to proteins of the type collagen or elastin, these instant AGE act as ligands for RAGE-receptors and provoke an inflammatory process. RAGE-receptors support cell in an enabled state, causing short-term anti-inflammatory response becomes a long cellular dysfunction.
АGE-Poduct and the receptor (RAGE): from vessels to Alzheimer's.
Receptor glycosylation end products (RAGE) is multiligand transmembrane glycoprotein type I, belonging to the superfamily of immunoglobulin (Ig). RAGE may participate in several pathological processes including diabetes, Alzheimer's disease (AD), systemic amyloidosis, and tumor growth.
RAGE was originally characterized based on its ability to bind AGEs, adducts formed by non-enzymatic glycosylation and oxidation of proteins and lipids. This process occurs in normal aging process and dramatically accelerated in diabetes, where hyperglycemia is the main trigger. Substantial evidence support a role for interaction of AGE/RAGE in the pathophysiology of diabetes. Both AGEs and RAGE are elevated in diabetes in the blood vessels, monocytes and podocytes.
RAGE may also mediate physiological functions such as neuronal growth, survival and regeneration, and plays an important role in proinflammatory reactions. RAGE is expressed at a high level in the development process, especially in the Central nervous system (CNS). It is also expressed at a lower level in adult cells: endothelial cells, including smooth muscle cells, mononuclear phagocytes, pericytes, neurons, cardiomyocytes, and hepatocytes. RAGE ligands include the end products of glycation (AGEs), protein amyloid-β (Aß), HMG-1 (also known as amphoteric) and several members of superselective protein S100.
Blockade of RAGE activation of recombinant sRAGE or blocking the function of antibodies reduces vascular permeability, the development of atherosclerotic lesions and enhances wound healing in patients with diabetes mellitus rodents. RAGE-null mice with diabetes do not develop signs of nephropathy, including increased expansion of mesangial matrix and thickening of glomerular membrane.
In contrast, transgenic overexpression of RAGE leads to the aggravation of diabetic nephropathy and retinopathy. RAGE is also a receptor for β-pleated fibrils, structures that are characteristic of amyloid. Aß is the main component of neurodegenerative plaques associated with Alzheimer's disease (AD) and RAGE colocalized with Aß in the brain of patients with asthma at increased amounts.
Sixty five million one hundred fifty five thousand one hundred seventy two
From a molecular point of view, Alzheimer's disease is characterized by deposits of abnormally aggregated proteins. In the case of extracellular amyloid plaques, these deposits mainly consist of filaments of β-amyloid peptides (Aß), in the case of the intracellular neurofibrillary tangles (NFT), mainly of protein tau.
AD is also characterized by increased expression of RAGE in neurons. RAGE is a receptor of the immunoglobulin family that has many ligands, which functions as the transmitting signal of the acceptor Aß on the cell surface. Receptor glycosylation end products (RAGE), which localized not only to neurons, astroglia and microglia, but also on endothelial cells, where it acts as a Transporter of beta-amyloid in the brain from the bloodstream.
Several groups shown that infusion of Aβ40 in mice leads to vasoconstriction of cerebral vessels and weakening of cerebral circulation (CBF). Patients with AD also have poor cerebral circulation. In AD mouse models in which transgenic animals sverkhekspressiya amyloid precursor protein (APP), which leads to disease causing plaque formation, it is demonstrated that RAGE is implicated as a pathogenic factor in the progression of the disease.
It is shown that RAGE binds to Aß-peptides. Inhibition of this interaction suppresses accumulation of Aß in transgenic animal models; therefore, I believe that RAGE is implicated in AD. It is shown that the treatment with sRAGE (soluble RAGE), and anti-RAGE-antibody reduces the number of plaques (Deane et al, 2003). Blocking the interaction of RAGE with amyloid with antibodies can be a suitable method for the treatment of patients with AD; however, the existing polyclonal antibodies obtained from the serum of animals, are not suitable for chronic treatment of humans.published
Author: Andrey Blueskin
See also:
Antiparasitic cleansing and priming
You can treat the nervous system, and hypertension and get a stroke because of ostechondrosis!
P. S. And remember, only by changing their consumption — together we change the world! ©
Join us in Facebook , Vkontakte, Odnoklassniki
Source: www.beloveshkin.com/2016/05/glikirovanie-i-metabolicheskaya-pamyat-mest-podaetsya-kholodnoj.html