699
Side effects of laser vision correction
In the 90s the cornea researched ultrasonic "pencil". Instead of a full map of the cornea was 10-15 measurements on the eye, which the surgeon made a mental idea of what is there in the patient. In 92-m to year spread topographers based on Placido.
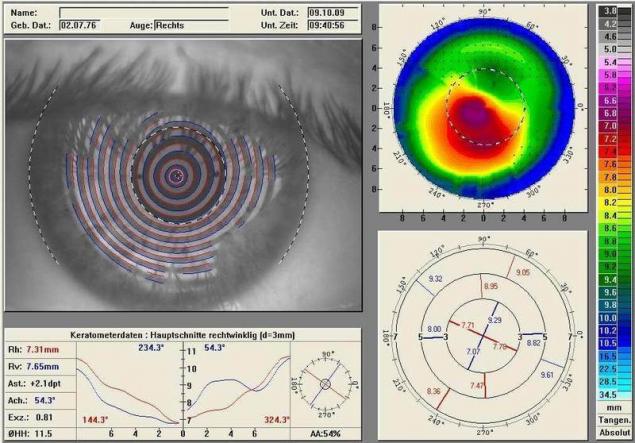
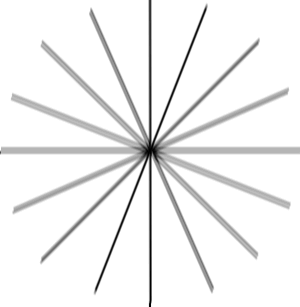
The idea is that if you make the projection of the light rings on the cornea, then they will be perfect round, as any distortion will give a distortion of the circle. That is, we had such a target in the eye in the ideal case, and the egg with astigmatism. And I watched, the light beam through the disk Placido. Now these disks have many surgeons in my pocket just in case.
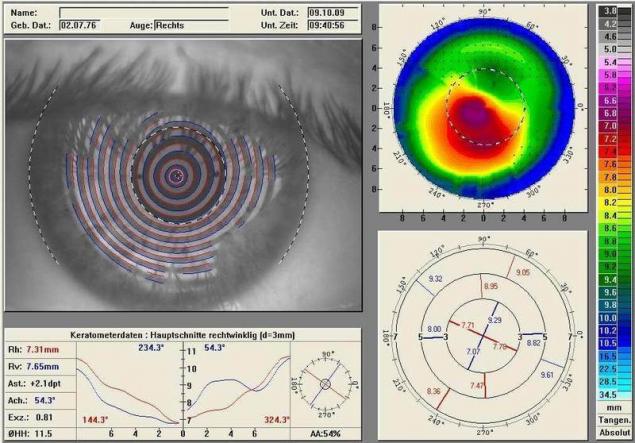
The method was, of course, very approximate. Then came automation: these disks have been in the 32-36 rings instead of 8 or 10, and the apparatus being photographed, and then recognized and expected distortion, and gave "depth map" of the eye.
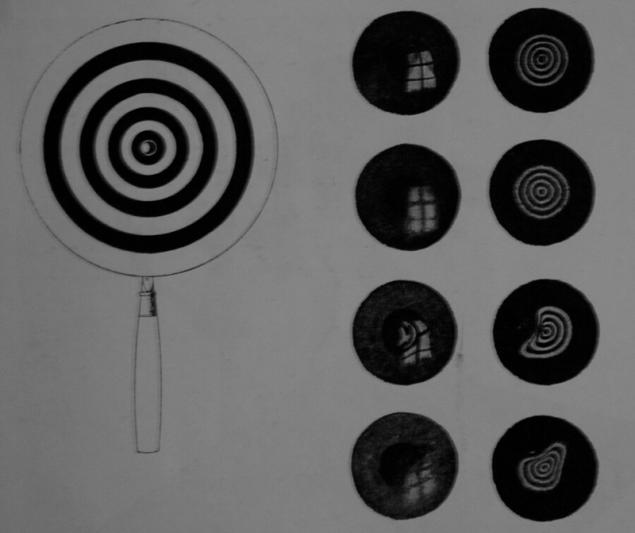
Here's a "target"
"The depth map" of the eye
At the same time for the diagnosis of keratoconus was important to measure the cornea not from above but from the side, and in parallel developed technology surveyor of Orbscan. Is profile reflectii there went the beam at the slit lamp (as in a scanner for papers), and it is possible to obtain optical media of the cornea, in particular, the back of her hand.
Accordingly, it has automated and made a sort of measuring in the tens of slices, and then assembling into a single map. As computed x-ray tomography, and in the light.
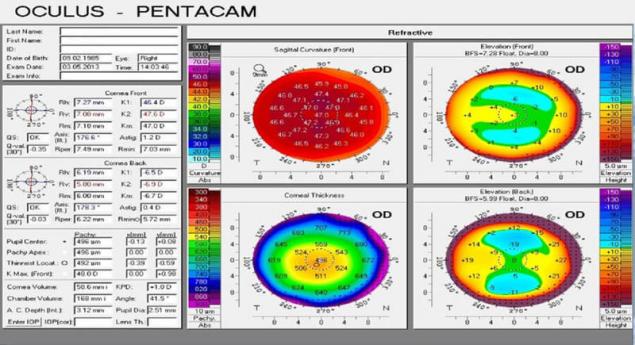
The next stage of evolution was the principle Hinflug, that is, the rotating beam. As you can guess from the name, invented it in Germany, and in the same city, where sits the Lake and the Oculus.
To date, the implementation of this principle, the unit "Pentacam" — the most popular diagnostic equipment for refractive surgery. A lot of information to 4 or 5 other devices assembled in one: here the thickness, the front surface, rear, depth of the anterior chamber. And this device is still evolving and becomes more accurate.
But the system, Placida died. In the case of complex patients, it includes information about the condition of the cornea. In this case, the system Placido good, because the surface topography after complications allows to build a map of the lifting surface to a perfect "target", i.e. to quickly calculate the difference between what is seen and what must be done, and then a laser to remove excess tissue.
This so-called topoguided-operation. Uneven cornea can result in more-less decent condition. Approximately the same principle applies superLASIK, which is customized for each individual patient every time. Analog — technique Custom Vue is wavefront-guided laser.
Here, the idea that the measured wavefront of the eye, and then an excimer laser destroys the essential part of the cornea. The method has pros and cons. Cons associated with what part of the distortion comes from the lens, to laser correction with the lens, nothing to do. The lens over the lifetime varies greatly, and the cornea is almost unchanged. He grows all his life.
Accordingly, supercircle in this case, enough for a couple of decades, young life... the result is now much more commonly used "ideal" profile for a cornea that is not associated with the current profile of the lens.
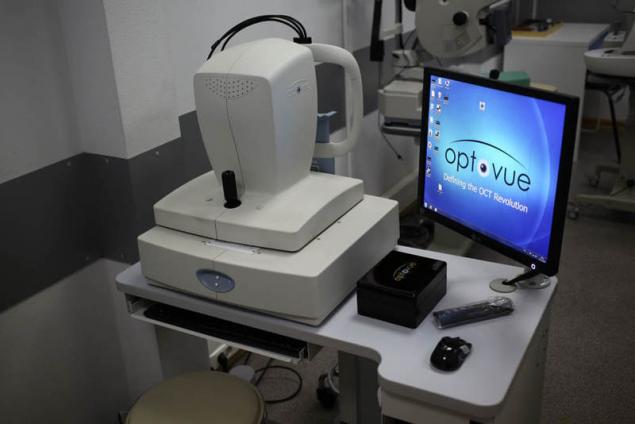
And there are also classic OCT (tomography) — it better shows the thickness of the fabric, and it is used additionally with corneal opacity precluding other methods.
Therefore, the results of selected diagnostic profile. In the case of modern operations, the surgeon builds a profile likeness of the wizard, entering the required data. Math for aspherical lens makes the firmware of the laser, the surgeon then selects from multiple possible results, or simply confirms the circuit operation.
Here ultrasonic "pencil":

The rest of the modern — at the end of the article. Meanwhile, important practical things for the operation.
We do not look through the center of the pupil
The next thing we want is centration of the cornea under the laser. The surgeon selects a cone for pneumatic auto — there are three sizes for different tasks. For myopia most often is the smallest, it lies on the periphery of the cornea.
The minimum number of people are looking through the center of the pupil. Usually our optical axis is slightly displaced toward the nose is the angle Kappa. Have hypermetropia (people with severe far-sightedness, for example), this angle more. Comes to what they watch sometimes on the very edge of the pupil.
So as not to cut the lens where it's not necessary, it is important to perform the centration on the optical axis. Therefore, the patient looks at a flashing led. But actually, of course, the patient we are here not trust completely, and be sure to control the capture of the Purkinje reflex.
I mean, with the glare, and not a conditioned response. This is the highlight that you know well on "red eyes" in photos with flash, only it can be shrunk almost to the point. It's not the axle itself, but it is located to the reflex very close, so that you can take this point over the center of the lens. In complex cases, sometimes between the center of the pupil and the reflex point is selected — it all depends on the provisional diagnosis.
This place is a support beam marked the centre ablation. Then turn on the laser. In excimer lasers have a high-speed camera, which monitors micro-movements of the eye and moves the laser in concert with them.
On older models the lasers during surgeries if the patient looked in the direction of the laser beat is not there. Since 2005, about the following the eye move with the beam. In the case of FLEX or SMILE when used femtosecond laser, the eyes just captured in pnevmoservis. Tracker is not there, but there is a gauge loss of vacuum before the eyes sucks, the laser will turn off.
The correct grip does not always happen. If so, the surgeon conducting decorrencia turn or recapture. Control grip is the overlap of the two images — from the camera in real time and with calibration to capture. Someday we will have avtosistemy, which will overlay the two images and capture correctly automatically. Today it depends on the experience of the surgeon.
Professor Secunda did a study — he compared 36 patients with and 36 femptoLASIK with a SMILE — location of the evacuation zone of the tissue in the second case was better. Even in the old MEL-80 (the most modern at the time).
Excimer laser have a lot to forgive an inexperienced surgeon. But an experienced surgeon can on VisuMAX to create a centration better than the conventional excimer automatically. Perhaps in the future there will be firmware and a manipulator that will reduce this factor of experience and skill of the surgeon.
In Istanbul was once a very complex patient with two decentrally close to strabismus. With him was quite difficult because we had to go through the language barrier, but in the end everything worked out. However, if possible, we always recommend to choose for complicated cases the surgeon, speaking the same language with you.
What is most important in the correction of astigmatism
So the world sees people with astigmatism:
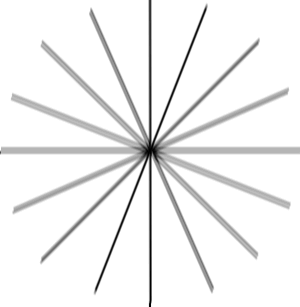
Simplifying what a healthy person would give a point on the retina, astigmatism becomes the ellipse or "eight" at a certain angle. Given this angle and the relative size of this distortion, it is possible to make lenses for glasses that have curvature will change the nonlinear compared with conventional lenses for myopia or hyperopia.
Some time later I learned to do the same contact lenses (it is important to insert in the eye without rotation), and then calculate the profiles to a "contact lens" to cut directly on the cornea or inside it. That is, to solve the General problem of laser vision correction.
Astigmatism corrected laser methods very effectively. However, the most difficult part — matching future profile of the lens and the eye. The fact is that if you miss with a twist on the 10% are lost the effect on the third. If the miss is 30%, the effect is completely come to naught.
In the end, the important part when working with the astigmatism becomes capturing the eye on the vacuum "sucker" of the laser. It is a matter of experience of the doctor (fortunately, do not have manual, so I do it almost everywhere and good). Modern lasers have the ability to deploy capture "inside", just rotating the patient's eyes — in the Indian research center has been proven to do so safely.
How is the laser focus through the lens fluid on the corneal surface and the microdroplets of fat?
When is the premedication analgesic (usually alcaina) on the surface of the eye gets a lot of drops. Then the eye at least once is wiped with a wet swab just before contact with pnevmatikatos laser. If the eye is dry, between the cone of the laser and the cornea are formed gaps, which would distort the focus.
If the eyes are wet, the liquid fills them, and spurious refractions is almost there. Miracal fat rounded up during the seizure due to the pressure. In the end, of course, still medium is formed is not perfect, and this is partly one of the reasons why lenticule should be bypassed with a spatula from both sides, separating it from the top and bottom layer of the cornea.
Significant error may be this: the eyelashes secrete oil that starts quickly and uncontrollably spread out over the surface. This fat breaks focus and remain major bridges that need to be split with a sharp spatula (as was done on last generation lasers) — or we need to abort at the sight of such a problem.
In our clinic we don't leave anything to chance, using a number of necessary manipulations: aspirators for the removal of excess fluid and fat droplets, special hygroscopic sponges, can even deprive you of a couple of lashes near the Central part of the eye — we'll cut in the event that they suddenly bulged out as not necessary.
How should the surgeon during the operation?
Not worth it, and sits. All eye surgery are made strictly sitting, so the hand moves a lot more stable. Righties work right from the patient, lefties on the left. Accordingly, an incision for the extraction of lenticule done where the surgeon is most convenient to access, closest to his hand with the tool. Why is it so important, I'll show you later when we will talk about what is in the operating room.
What are the complications the most severe?
Complications of LASIK to 6% on technique and FLEX — up to 2%, on SMILE — 0,5-1% (depends on the generation lasers, 0,5% is the sixth). The last number is not confirmed by decades of clinical trials — the data will be officially published until the summer of 2017, but you can like according to Wikipedia — in articles about the different methods are quite rich in references to research.
One of the worst complications of any correction also PRK — keratectasia (when the cornea bulges, as in keratoconus). The result of the operation it can happen due to a substantial violation of the biomechanics of the eye, usually either because of incomplete diagnosis, or because of surprise, which means the diagnosis of the doctor was not able to identify. It is therefore important to make the diagnosis very thoroughly and different methods.
I must admit that on the most expensive "reinsurance" equipment in hospitals are often save. On the other hand, if the patient comes with keratectasia, then it is likely to be direct testimony to the good old PRK. Generally, any thin corneas, but still not quite smooth — its okay dub PRK.
In the early stages of keratoconus PRK levels the surface and once on top we still doing cross-linking (treatment with a high content of B12, then the release of oxygen by laser heating and fixation of the collagen in ultraviolet — all to make it hard, but about that later separately). This niche will provide life PRK another 10 years at least.
Keratoconus is a difficult complication in the medium order. Once done cross-linking, that is, kartaltepe treated as usual. Can be inserted vnutribronhialno washer.
Historically, part of keratectasia after SMILE are cases when the surgeon found patient's cornea and decided not to do an invasive procedure LASIK or a derivative thereof, but for some reason decided that ReLEx can "ride" because of the low invasiveness. No. The patient's cornea is not necessary to adjust without reinforcement. You can do cross-linking, rings, transplantation.
Next in popularity we have detached the flap after LASIK, technique or FLEX. Often, of course, get LASIK — they the total risk of different side effects at 6%, while their country do a lot even still.
Any patchwork methods of correction is a contraindication to contact sports. You can give birth, but to "in your face" — is undesirable. There were cases when the flap tore from the fact that the child is just sloppy poked his mother in the face, from the fact that the woman caught the eye stick for tomatoes in General, very different.
Let me remind you, the problem is that when these methods cut a "lid" which "leans" to create a lens inside the cornea, and then this "lid" is closed back. Eye associates her thin jumper-the"loop" and accrued on top of a thin layer of epithelium. Flap is not incremented and kept, not opening, only through the surface epithelium on top.
Flap LASIK can be removed at least 8-10 years (there were cases) — and disperse it in exactly the same place on the day of surgery. In the case of the technique and FLEX flap holds stronger, there is often scarring around the edges (thin white stripes) — 2-3 years already, you can try to tear it with his teeth, and he will not give in.
In the case of SMILE flap at all, but there is a "tunnel" (cut at 2.5 mm), through which goes lenticule from the cornea — it is also covered with epithelium, but before it is overgrown, it is impossible to wash, so as not to contaminate it. Our colleague from Ekaterinburg, told about a patient with a SMILE, who was severely beaten — damage passed on eye is very extensive, but the weakest point was not in the correct place.
Eyes managed to save, sees the patient well. Or rather, began to see, in a couple of weeks. A similar case was in the practice of the bloom (second inventor of the technology correction). In Germany now for work in the police, you can only do PRK in 13 of the 16 Federal States. Three more allowed technique.
Contrary to popular myth, Romanova membrane, which is located on top of the cornea (which is destroyed when PRK and severely injured when technique-methods) does not give protection against mechanical damage impact. It ensures the stability of the "slow" type, in particular, compensates the pressure inside the eye.
Now it is necessary to talk about the halo effect is a halo around lights at night. It can give any laser correction. It depends on the magnitude of the correction zone in relation to the pupil. A common area of correction — 7 millimeters.
The eyeball some people have revealed up to 8 millimeters in the dark. Before doing the correction zone 4-5 millimeters. The second reason for the halo (more relevant to modern operations) is how flat your cornea in the center. The center must rise (a healthy cornea has a center diopter more than the edges — for example, 38 D in the center, 42 D on the edges).
Good Pro calculates the cutting profile to the laser so that the cornea is flattened over a large area. Excimer lasers have different aspherical profiles for this. ReLEx SMILE itself aferican on the architecture of the intervention. Yes, the natural condition of the cornea worsens in any correction, but SMILE — less.
Then we have the photophobia and the overgrowth of the tissues. Problem medication. In PRK Russia has not used the "normal" for this operation, mutamycin (he's not allowed at the state level). Analogs slightly riskier. Now, ophthalmologists are trying to lobby for the resolution of this product for operations.
Another case of incomplete extraction of lenticule when you SMILE-operation. Were extremely rare cases where there was a part that was impossible to pick up with tweezers. In this case, the injected cortisone, which stains a small piece and then you can go inside and retrieve it.
In London one of the very expensive surgeons makes the second cut at this event in front of the first he never uses but keeps in case of problems during operation. Usually if the laser didn't cut something in lenticule is a problem of the surgeon, which for some reason climbed up and tried to useprivate the place where it was not cut. That's right — give heal to do PRK topography. Or, alternatively, go to FLEX instead of SMILE.
Then tear the edges of incizii — a very unlikely thing in experienced hands, when a surgeon tool breaks the entrance to the tunnel leading to lenticule. To happen in practice, it is necessary to push him in the shoulder during the operation. However, problems are usually not: there was a slit of 3 mm, a 3.5 mm is nothing really.
In the vast majority of cases incision toiling radially, but there was one example at the beginning of the history of corrections when there was a strain of 1.5 mm towards the center. From the area of 7.8 mm it turned out area of 6.8 mm, the patient received a halo effect in the deep dark. The solution is simple — a second hand is necessary to keep the eye with a tweezer, since this is a mandatory Protocol SMILE.
Serious (but fortunately reversible) it should be noted keratitis. It is an inflammation of the cornea, most commonly the result of infections. Its three stages — the second is usually cortisone and treatment at the discretion of the physician, and in the third — be sure to rinse the pocket (there is a risk of permanent scarring). So after the surgery you see the next day and again and again.
Everything else usually passes within a week or two after surgery and is associated with the body's response to mechanical tissue damage or features of the medications. Yes, you can cry for a couple of hours, Yes, it can sting, Yes, someone has analgesic causes then a wild desire of the honour of eye (what not to do). And Yes, the first couple of days you'd better not get in a beauty contest and shoot portraits for a Dating site. Then all will be well.
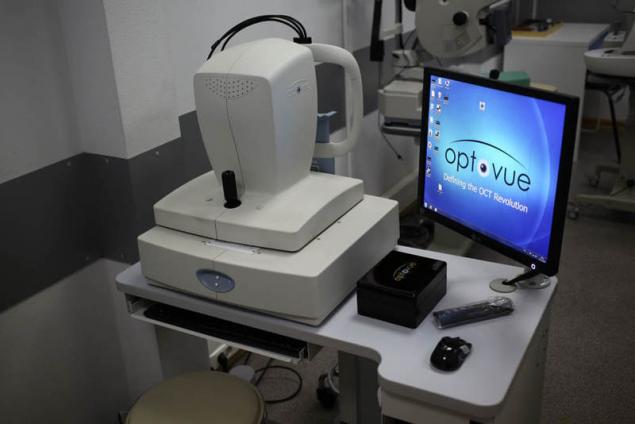
Diagnostic equipment
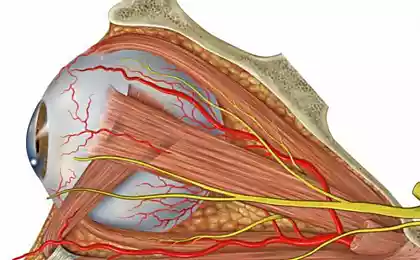
Spectral optical coherence tomography — high-frequency contactless method of diagnostics of the morphology of the cornea, retina and optic nerve. During the procedure uses laser beam or infrared light. The result of the OCT is two-dimensional or three-dimensional picture:
Pentacam — the "gold standard" in the diagnosis of diseases of the cornea.

Rotary Hinflug camera for computerized topography of the cornea and comprehensive study of the anterior segment of the eyeball. Automatically calculates important parameters such as the curvature of the anterior and posterior surfaces of the cornea, the total optical power of the cornea, pachymetry, anterior chamber depth, anterior chamber angle in 360°, and the densitometry of the cornea and lens.
Contactless measurement takes 1-2 seconds and includes Simply 25 or 50 images (depending on scanning mode). In sum, to build a 3D model of the anterior segment of the eye are detected and analyzed to 25000 real elevation points. Automatic control system guidance provides ease of measurement and high repeatability of results.
The view from the side of the doctor:

Left — auto-auto Ref-kerato meter based on the use of special wavefront sensor Hartmann-Shack, which allows pointwise to analyze the wavefront reflected from the retina light. Using the analysis of the wave front, we can analyze the aberrations of the ocular system and to choose the best correction. Right automatic non — contact pneumotonometer, allows to measure intraocular pressure and corneal-compensated intraocular pressure.
The view from the side of the patient:

Left — automatic touchless pneumotonometer.
Right auto autorefkeratometer.
Automatic sign projector can be mounted on the wall or on the table. Works for distances from 2.5 to 8.0 meters. Equipped with a remote control. Contains over 40 of the most essential tests, including for children. The high speed of the slideshow (0.15 seconds). High resolution (50 lines / mm) allows to accurately assess the visual acuity of the patient:

The diagnostics for comprehensive diagnosis of pathology of the anterior and posterior segment of the eye, you can see the projector:

Automated perimeter — visual field analyzer:

Is used to determine the threshold sensitivity of the retina of the organ of vision, revealing pathological changes in the early stages.
Optical coherence tomography (OCT):

OST Is a method of displaying structure of biological tissues in cross-section with a high level of resolution.
The diagnostics for the initial diagnostic examination:

Optical iolmaster IOL Master 700 is the new generation gold standard in optical biometry:

Optical device for contactless measurement of ocular structures using the method of optical coherence tomography. Optical biometrics with a new generation of technology Swept Source OCT provides anterior and posterior segment of the eye. This not only allows a better understanding of the surgical anatomy of the eye, but more accurately calculate the refractive result of the surgery.
Automatic lensmeter is the optimal device for the selection of the points of evaluation of the quality of the lens, removing the prismatic testimony:

IOL-Master 500 — simple and perfect. With it for a few seconds produced the most precise measurements of biometric parameters of the eye required for calculating IOL (intraocular lenses):

Especially valuable is that the measurements are carried out in a contactless manner. With one click you can quickly obtain accurate data on the length of the anteroposterior axis of the eye, the radius of curvature of the cornea, its diameter and the depth of the anterior chamber.
Slit lamp with video camera — a device that under magnification to inspect the visible parts of the eye such as the eyelid, sclera, conjunctiva, iris, lens and cornea:

With the help of special lenses at the slit lamp visible of the Central and peripheral parts of the fundus. Slit lamp consists of a binocular microscope and a source of narrow light. Examination with slit lamp biomicroscopy is the eye. The photo - and video-taking.
Aberrometer — wavefront analyzer, using the Fourier algorithms, it reflects the unique flaws a patient's eye using 100 percent of the available points in Hartmann-shark for a more accurate determination of wavefront errors:

The system provides the highest resolution available for any pupil size, allowing precise, individual approach for a wide range of optical errors.
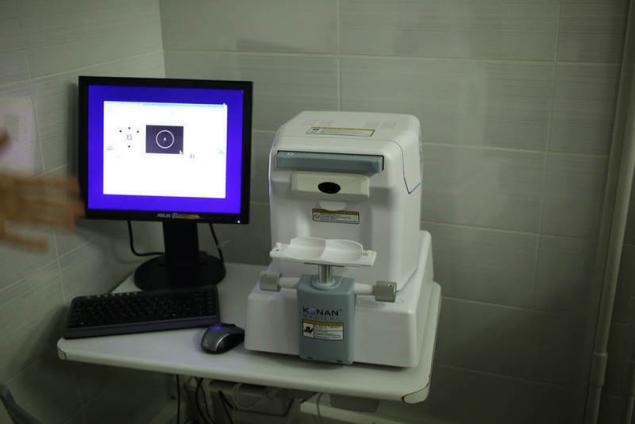
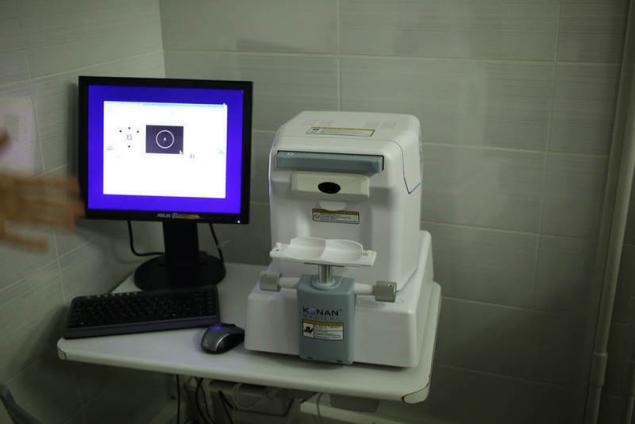
The endothelial microscope is required for observation and analysis of the endothelial layer of the cornea, measurement of corneal thickness and automatic photographing:
Digital fotodelika lamp is used to obtain digital images with high resolution, video. The software allows optimally organize computer processing and storage of digital images:

Office of primary diagnosis:

Contact tonometer the TONO-PEN is a lightweight and ergonomic device:

Despite its small size and weight, accuracy comparable to the Goldmann tonometer. The basis of TONO-PEN load cell with a diameter of the contact surface of 1.5 mm, almost imperceptibly touches the cornea and produces the arithmetic mean of results of four independent measurements and a statistical factor.published
Source: geektimes.ru/company/klinika_shilovoy/blog/284348/
The idea is that if you make the projection of the light rings on the cornea, then they will be perfect round, as any distortion will give a distortion of the circle. That is, we had such a target in the eye in the ideal case, and the egg with astigmatism. And I watched, the light beam through the disk Placido. Now these disks have many surgeons in my pocket just in case.
The method was, of course, very approximate. Then came automation: these disks have been in the 32-36 rings instead of 8 or 10, and the apparatus being photographed, and then recognized and expected distortion, and gave "depth map" of the eye.
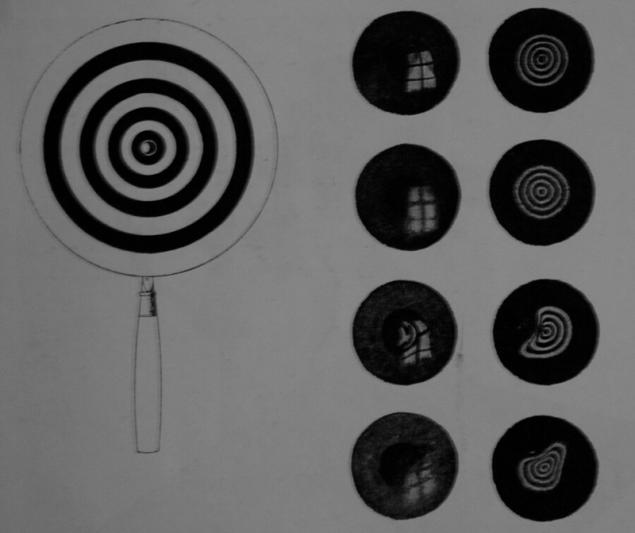
Here's a "target"
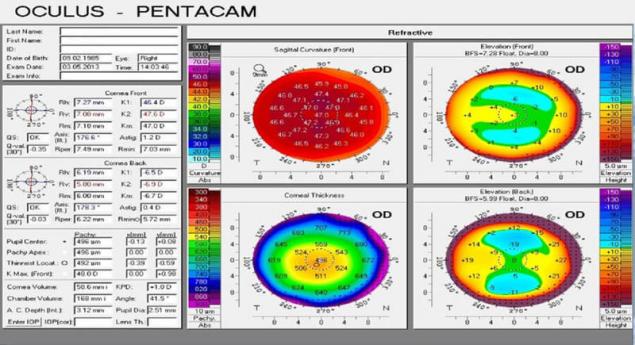
"The depth map" of the eye
At the same time for the diagnosis of keratoconus was important to measure the cornea not from above but from the side, and in parallel developed technology surveyor of Orbscan. Is profile reflectii there went the beam at the slit lamp (as in a scanner for papers), and it is possible to obtain optical media of the cornea, in particular, the back of her hand.
Accordingly, it has automated and made a sort of measuring in the tens of slices, and then assembling into a single map. As computed x-ray tomography, and in the light.
The next stage of evolution was the principle Hinflug, that is, the rotating beam. As you can guess from the name, invented it in Germany, and in the same city, where sits the Lake and the Oculus.
To date, the implementation of this principle, the unit "Pentacam" — the most popular diagnostic equipment for refractive surgery. A lot of information to 4 or 5 other devices assembled in one: here the thickness, the front surface, rear, depth of the anterior chamber. And this device is still evolving and becomes more accurate.
But the system, Placida died. In the case of complex patients, it includes information about the condition of the cornea. In this case, the system Placido good, because the surface topography after complications allows to build a map of the lifting surface to a perfect "target", i.e. to quickly calculate the difference between what is seen and what must be done, and then a laser to remove excess tissue.
This so-called topoguided-operation. Uneven cornea can result in more-less decent condition. Approximately the same principle applies superLASIK, which is customized for each individual patient every time. Analog — technique Custom Vue is wavefront-guided laser.
Here, the idea that the measured wavefront of the eye, and then an excimer laser destroys the essential part of the cornea. The method has pros and cons. Cons associated with what part of the distortion comes from the lens, to laser correction with the lens, nothing to do. The lens over the lifetime varies greatly, and the cornea is almost unchanged. He grows all his life.
Accordingly, supercircle in this case, enough for a couple of decades, young life... the result is now much more commonly used "ideal" profile for a cornea that is not associated with the current profile of the lens.
And there are also classic OCT (tomography) — it better shows the thickness of the fabric, and it is used additionally with corneal opacity precluding other methods.
Therefore, the results of selected diagnostic profile. In the case of modern operations, the surgeon builds a profile likeness of the wizard, entering the required data. Math for aspherical lens makes the firmware of the laser, the surgeon then selects from multiple possible results, or simply confirms the circuit operation.
Here ultrasonic "pencil":

The rest of the modern — at the end of the article. Meanwhile, important practical things for the operation.
We do not look through the center of the pupil
The next thing we want is centration of the cornea under the laser. The surgeon selects a cone for pneumatic auto — there are three sizes for different tasks. For myopia most often is the smallest, it lies on the periphery of the cornea.
The minimum number of people are looking through the center of the pupil. Usually our optical axis is slightly displaced toward the nose is the angle Kappa. Have hypermetropia (people with severe far-sightedness, for example), this angle more. Comes to what they watch sometimes on the very edge of the pupil.
So as not to cut the lens where it's not necessary, it is important to perform the centration on the optical axis. Therefore, the patient looks at a flashing led. But actually, of course, the patient we are here not trust completely, and be sure to control the capture of the Purkinje reflex.
I mean, with the glare, and not a conditioned response. This is the highlight that you know well on "red eyes" in photos with flash, only it can be shrunk almost to the point. It's not the axle itself, but it is located to the reflex very close, so that you can take this point over the center of the lens. In complex cases, sometimes between the center of the pupil and the reflex point is selected — it all depends on the provisional diagnosis.
This place is a support beam marked the centre ablation. Then turn on the laser. In excimer lasers have a high-speed camera, which monitors micro-movements of the eye and moves the laser in concert with them.
On older models the lasers during surgeries if the patient looked in the direction of the laser beat is not there. Since 2005, about the following the eye move with the beam. In the case of FLEX or SMILE when used femtosecond laser, the eyes just captured in pnevmoservis. Tracker is not there, but there is a gauge loss of vacuum before the eyes sucks, the laser will turn off.
The correct grip does not always happen. If so, the surgeon conducting decorrencia turn or recapture. Control grip is the overlap of the two images — from the camera in real time and with calibration to capture. Someday we will have avtosistemy, which will overlay the two images and capture correctly automatically. Today it depends on the experience of the surgeon.
Professor Secunda did a study — he compared 36 patients with and 36 femptoLASIK with a SMILE — location of the evacuation zone of the tissue in the second case was better. Even in the old MEL-80 (the most modern at the time).
Excimer laser have a lot to forgive an inexperienced surgeon. But an experienced surgeon can on VisuMAX to create a centration better than the conventional excimer automatically. Perhaps in the future there will be firmware and a manipulator that will reduce this factor of experience and skill of the surgeon.
In Istanbul was once a very complex patient with two decentrally close to strabismus. With him was quite difficult because we had to go through the language barrier, but in the end everything worked out. However, if possible, we always recommend to choose for complicated cases the surgeon, speaking the same language with you.
What is most important in the correction of astigmatism
So the world sees people with astigmatism:
Simplifying what a healthy person would give a point on the retina, astigmatism becomes the ellipse or "eight" at a certain angle. Given this angle and the relative size of this distortion, it is possible to make lenses for glasses that have curvature will change the nonlinear compared with conventional lenses for myopia or hyperopia.
Some time later I learned to do the same contact lenses (it is important to insert in the eye without rotation), and then calculate the profiles to a "contact lens" to cut directly on the cornea or inside it. That is, to solve the General problem of laser vision correction.
Astigmatism corrected laser methods very effectively. However, the most difficult part — matching future profile of the lens and the eye. The fact is that if you miss with a twist on the 10% are lost the effect on the third. If the miss is 30%, the effect is completely come to naught.
In the end, the important part when working with the astigmatism becomes capturing the eye on the vacuum "sucker" of the laser. It is a matter of experience of the doctor (fortunately, do not have manual, so I do it almost everywhere and good). Modern lasers have the ability to deploy capture "inside", just rotating the patient's eyes — in the Indian research center has been proven to do so safely.
How is the laser focus through the lens fluid on the corneal surface and the microdroplets of fat?
When is the premedication analgesic (usually alcaina) on the surface of the eye gets a lot of drops. Then the eye at least once is wiped with a wet swab just before contact with pnevmatikatos laser. If the eye is dry, between the cone of the laser and the cornea are formed gaps, which would distort the focus.
If the eyes are wet, the liquid fills them, and spurious refractions is almost there. Miracal fat rounded up during the seizure due to the pressure. In the end, of course, still medium is formed is not perfect, and this is partly one of the reasons why lenticule should be bypassed with a spatula from both sides, separating it from the top and bottom layer of the cornea.
Significant error may be this: the eyelashes secrete oil that starts quickly and uncontrollably spread out over the surface. This fat breaks focus and remain major bridges that need to be split with a sharp spatula (as was done on last generation lasers) — or we need to abort at the sight of such a problem.
In our clinic we don't leave anything to chance, using a number of necessary manipulations: aspirators for the removal of excess fluid and fat droplets, special hygroscopic sponges, can even deprive you of a couple of lashes near the Central part of the eye — we'll cut in the event that they suddenly bulged out as not necessary.
How should the surgeon during the operation?
Not worth it, and sits. All eye surgery are made strictly sitting, so the hand moves a lot more stable. Righties work right from the patient, lefties on the left. Accordingly, an incision for the extraction of lenticule done where the surgeon is most convenient to access, closest to his hand with the tool. Why is it so important, I'll show you later when we will talk about what is in the operating room.
What are the complications the most severe?
Complications of LASIK to 6% on technique and FLEX — up to 2%, on SMILE — 0,5-1% (depends on the generation lasers, 0,5% is the sixth). The last number is not confirmed by decades of clinical trials — the data will be officially published until the summer of 2017, but you can like according to Wikipedia — in articles about the different methods are quite rich in references to research.
One of the worst complications of any correction also PRK — keratectasia (when the cornea bulges, as in keratoconus). The result of the operation it can happen due to a substantial violation of the biomechanics of the eye, usually either because of incomplete diagnosis, or because of surprise, which means the diagnosis of the doctor was not able to identify. It is therefore important to make the diagnosis very thoroughly and different methods.
I must admit that on the most expensive "reinsurance" equipment in hospitals are often save. On the other hand, if the patient comes with keratectasia, then it is likely to be direct testimony to the good old PRK. Generally, any thin corneas, but still not quite smooth — its okay dub PRK.
In the early stages of keratoconus PRK levels the surface and once on top we still doing cross-linking (treatment with a high content of B12, then the release of oxygen by laser heating and fixation of the collagen in ultraviolet — all to make it hard, but about that later separately). This niche will provide life PRK another 10 years at least.
Keratoconus is a difficult complication in the medium order. Once done cross-linking, that is, kartaltepe treated as usual. Can be inserted vnutribronhialno washer.
Historically, part of keratectasia after SMILE are cases when the surgeon found patient's cornea and decided not to do an invasive procedure LASIK or a derivative thereof, but for some reason decided that ReLEx can "ride" because of the low invasiveness. No. The patient's cornea is not necessary to adjust without reinforcement. You can do cross-linking, rings, transplantation.
Next in popularity we have detached the flap after LASIK, technique or FLEX. Often, of course, get LASIK — they the total risk of different side effects at 6%, while their country do a lot even still.
Any patchwork methods of correction is a contraindication to contact sports. You can give birth, but to "in your face" — is undesirable. There were cases when the flap tore from the fact that the child is just sloppy poked his mother in the face, from the fact that the woman caught the eye stick for tomatoes in General, very different.
Let me remind you, the problem is that when these methods cut a "lid" which "leans" to create a lens inside the cornea, and then this "lid" is closed back. Eye associates her thin jumper-the"loop" and accrued on top of a thin layer of epithelium. Flap is not incremented and kept, not opening, only through the surface epithelium on top.
Flap LASIK can be removed at least 8-10 years (there were cases) — and disperse it in exactly the same place on the day of surgery. In the case of the technique and FLEX flap holds stronger, there is often scarring around the edges (thin white stripes) — 2-3 years already, you can try to tear it with his teeth, and he will not give in.
In the case of SMILE flap at all, but there is a "tunnel" (cut at 2.5 mm), through which goes lenticule from the cornea — it is also covered with epithelium, but before it is overgrown, it is impossible to wash, so as not to contaminate it. Our colleague from Ekaterinburg, told about a patient with a SMILE, who was severely beaten — damage passed on eye is very extensive, but the weakest point was not in the correct place.
Eyes managed to save, sees the patient well. Or rather, began to see, in a couple of weeks. A similar case was in the practice of the bloom (second inventor of the technology correction). In Germany now for work in the police, you can only do PRK in 13 of the 16 Federal States. Three more allowed technique.
Contrary to popular myth, Romanova membrane, which is located on top of the cornea (which is destroyed when PRK and severely injured when technique-methods) does not give protection against mechanical damage impact. It ensures the stability of the "slow" type, in particular, compensates the pressure inside the eye.
Now it is necessary to talk about the halo effect is a halo around lights at night. It can give any laser correction. It depends on the magnitude of the correction zone in relation to the pupil. A common area of correction — 7 millimeters.
The eyeball some people have revealed up to 8 millimeters in the dark. Before doing the correction zone 4-5 millimeters. The second reason for the halo (more relevant to modern operations) is how flat your cornea in the center. The center must rise (a healthy cornea has a center diopter more than the edges — for example, 38 D in the center, 42 D on the edges).
Good Pro calculates the cutting profile to the laser so that the cornea is flattened over a large area. Excimer lasers have different aspherical profiles for this. ReLEx SMILE itself aferican on the architecture of the intervention. Yes, the natural condition of the cornea worsens in any correction, but SMILE — less.
Then we have the photophobia and the overgrowth of the tissues. Problem medication. In PRK Russia has not used the "normal" for this operation, mutamycin (he's not allowed at the state level). Analogs slightly riskier. Now, ophthalmologists are trying to lobby for the resolution of this product for operations.
Another case of incomplete extraction of lenticule when you SMILE-operation. Were extremely rare cases where there was a part that was impossible to pick up with tweezers. In this case, the injected cortisone, which stains a small piece and then you can go inside and retrieve it.
In London one of the very expensive surgeons makes the second cut at this event in front of the first he never uses but keeps in case of problems during operation. Usually if the laser didn't cut something in lenticule is a problem of the surgeon, which for some reason climbed up and tried to useprivate the place where it was not cut. That's right — give heal to do PRK topography. Or, alternatively, go to FLEX instead of SMILE.
Then tear the edges of incizii — a very unlikely thing in experienced hands, when a surgeon tool breaks the entrance to the tunnel leading to lenticule. To happen in practice, it is necessary to push him in the shoulder during the operation. However, problems are usually not: there was a slit of 3 mm, a 3.5 mm is nothing really.
In the vast majority of cases incision toiling radially, but there was one example at the beginning of the history of corrections when there was a strain of 1.5 mm towards the center. From the area of 7.8 mm it turned out area of 6.8 mm, the patient received a halo effect in the deep dark. The solution is simple — a second hand is necessary to keep the eye with a tweezer, since this is a mandatory Protocol SMILE.
Serious (but fortunately reversible) it should be noted keratitis. It is an inflammation of the cornea, most commonly the result of infections. Its three stages — the second is usually cortisone and treatment at the discretion of the physician, and in the third — be sure to rinse the pocket (there is a risk of permanent scarring). So after the surgery you see the next day and again and again.
Everything else usually passes within a week or two after surgery and is associated with the body's response to mechanical tissue damage or features of the medications. Yes, you can cry for a couple of hours, Yes, it can sting, Yes, someone has analgesic causes then a wild desire of the honour of eye (what not to do). And Yes, the first couple of days you'd better not get in a beauty contest and shoot portraits for a Dating site. Then all will be well.
Diagnostic equipment
Spectral optical coherence tomography — high-frequency contactless method of diagnostics of the morphology of the cornea, retina and optic nerve. During the procedure uses laser beam or infrared light. The result of the OCT is two-dimensional or three-dimensional picture:
Pentacam — the "gold standard" in the diagnosis of diseases of the cornea.

Rotary Hinflug camera for computerized topography of the cornea and comprehensive study of the anterior segment of the eyeball. Automatically calculates important parameters such as the curvature of the anterior and posterior surfaces of the cornea, the total optical power of the cornea, pachymetry, anterior chamber depth, anterior chamber angle in 360°, and the densitometry of the cornea and lens.
Contactless measurement takes 1-2 seconds and includes Simply 25 or 50 images (depending on scanning mode). In sum, to build a 3D model of the anterior segment of the eye are detected and analyzed to 25000 real elevation points. Automatic control system guidance provides ease of measurement and high repeatability of results.
The view from the side of the doctor:

Left — auto-auto Ref-kerato meter based on the use of special wavefront sensor Hartmann-Shack, which allows pointwise to analyze the wavefront reflected from the retina light. Using the analysis of the wave front, we can analyze the aberrations of the ocular system and to choose the best correction. Right automatic non — contact pneumotonometer, allows to measure intraocular pressure and corneal-compensated intraocular pressure.
The view from the side of the patient:

Left — automatic touchless pneumotonometer.
Right auto autorefkeratometer.
Automatic sign projector can be mounted on the wall or on the table. Works for distances from 2.5 to 8.0 meters. Equipped with a remote control. Contains over 40 of the most essential tests, including for children. The high speed of the slideshow (0.15 seconds). High resolution (50 lines / mm) allows to accurately assess the visual acuity of the patient:

The diagnostics for comprehensive diagnosis of pathology of the anterior and posterior segment of the eye, you can see the projector:

Automated perimeter — visual field analyzer:

Is used to determine the threshold sensitivity of the retina of the organ of vision, revealing pathological changes in the early stages.
Optical coherence tomography (OCT):

OST Is a method of displaying structure of biological tissues in cross-section with a high level of resolution.
The diagnostics for the initial diagnostic examination:

Optical iolmaster IOL Master 700 is the new generation gold standard in optical biometry:

Optical device for contactless measurement of ocular structures using the method of optical coherence tomography. Optical biometrics with a new generation of technology Swept Source OCT provides anterior and posterior segment of the eye. This not only allows a better understanding of the surgical anatomy of the eye, but more accurately calculate the refractive result of the surgery.
Automatic lensmeter is the optimal device for the selection of the points of evaluation of the quality of the lens, removing the prismatic testimony:

IOL-Master 500 — simple and perfect. With it for a few seconds produced the most precise measurements of biometric parameters of the eye required for calculating IOL (intraocular lenses):

Especially valuable is that the measurements are carried out in a contactless manner. With one click you can quickly obtain accurate data on the length of the anteroposterior axis of the eye, the radius of curvature of the cornea, its diameter and the depth of the anterior chamber.
Slit lamp with video camera — a device that under magnification to inspect the visible parts of the eye such as the eyelid, sclera, conjunctiva, iris, lens and cornea:

With the help of special lenses at the slit lamp visible of the Central and peripheral parts of the fundus. Slit lamp consists of a binocular microscope and a source of narrow light. Examination with slit lamp biomicroscopy is the eye. The photo - and video-taking.
Aberrometer — wavefront analyzer, using the Fourier algorithms, it reflects the unique flaws a patient's eye using 100 percent of the available points in Hartmann-shark for a more accurate determination of wavefront errors:

The system provides the highest resolution available for any pupil size, allowing precise, individual approach for a wide range of optical errors.
The endothelial microscope is required for observation and analysis of the endothelial layer of the cornea, measurement of corneal thickness and automatic photographing:
Digital fotodelika lamp is used to obtain digital images with high resolution, video. The software allows optimally organize computer processing and storage of digital images:

Office of primary diagnosis:

Contact tonometer the TONO-PEN is a lightweight and ergonomic device:

Despite its small size and weight, accuracy comparable to the Goldmann tonometer. The basis of TONO-PEN load cell with a diameter of the contact surface of 1.5 mm, almost imperceptibly touches the cornea and produces the arithmetic mean of results of four independent measurements and a statistical factor.published
Source: geektimes.ru/company/klinika_shilovoy/blog/284348/