Part 4.2 of sight returns. From points to the excimer laser
Guys, there's a laser. He bites into your eyes. But before that the laser could begin, it was necessary to carefully clean up the eyes with a scalpel. Scalpel eventually becomes smaller, and the laser - steeper. So let's look at the evolution of methods. Blockquote> The epigraph from Milfgard

The final part of the cycle devoted itself remains the method of vision correction. In this section we consider the orthokeratology, all variants of laser vision correction, lens replacement and a few other methods. If you have not read the series from the start, I highly recommend to get acquainted with parts 2 and 4.1, which discusses in detail the problems faced by modern ophthalmic surgeon. In this article I will try to dispel already podnadoevshy fear associated with the movie "Final Destination 4" and a crazy laser. Also I will try to answer the questions asked readers, as promised.
The previous part h4> Part 1. Unboxing VisuMax - femto laser vision correction
Part 2. How many megabits / sec can be sent through the optic nerve and retina at what resolution? Some theory
Part 3. Meet - laser named Amaris. Removals and first awakening VisuMax
Part 4.1 restored sight. From points to the excimer laser
Contents:
Change the cornea
History: Radial keratotomy Swifts lawn or how to get to the work area PRK PRK and trans LASIK < femto-LASIK ReLEx SMILE ReLEx Flex Orthokeratology When the cornea is not enough
Implantation of phakic lens Implantation of artificial lenses - IOL
Change the cornea h4> exhausted all possibilities of time correction of various lenses, go to the methods. which will allow to remove all points. Most often an indication for laser vision correction is the desire of the patient to get rid of glasses. Sometimes it is a medical condition associated with complex types of astigmatism and myopia, which are difficult to correct in other ways. Many techniques, but they all boil down to reshape the cornea in order to correct the refraction of light.
For a more complete understanding of the techniques we turn to the structure of the cornea.
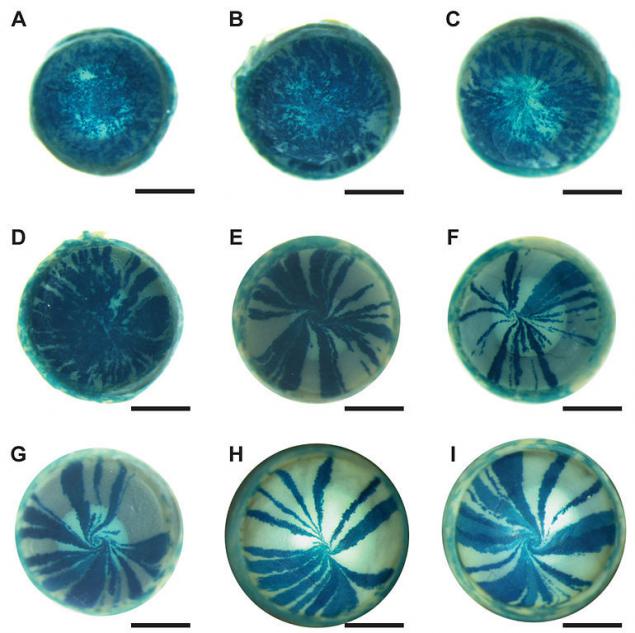
The first protective barrier between the eye tissues and the external environment is a anterior epithelium Photos mutant mice showing the regeneration of the epithelium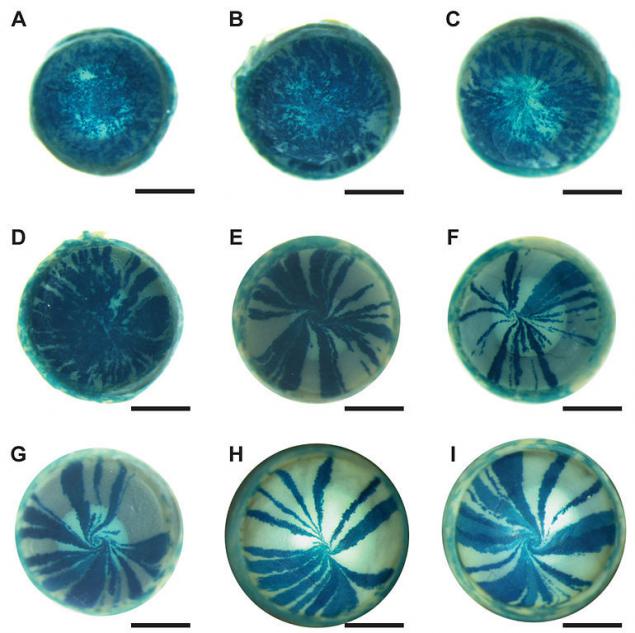
"Mosaic analysis" updates epithelial stem cells in the eye of the mouse. Applied staining using the reporter gene encoding the beta-galactosidase protein. Half of the cells of the body in this mouse model ekpressiruet transgene XLacZ, half - no. The photographs of different eye "mosaic" of mice can be observed, as new cells are pushed toward the center, creating a small "whirlpool." A: Three weeks after birth, stem cells are only beginning to be activated; B: 6 weeks; C: 8 weeks; D: 10 weeks; E: 15 weeks; F: 20 weeks; G: 26 weeks. Detail of illustration of Mort et al., 2009.
The next layer - Bowman's membrane The most important layer in terms of vision correction - stroma
History: Radial keratotomy h4>
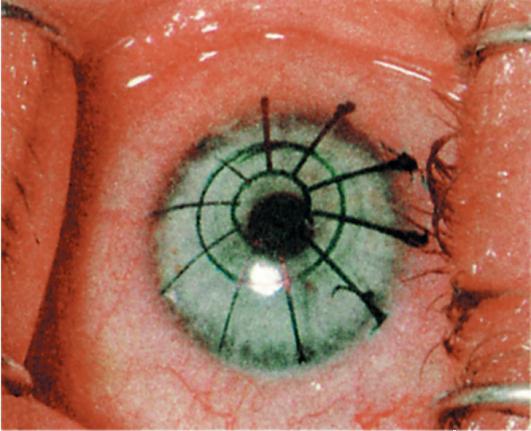
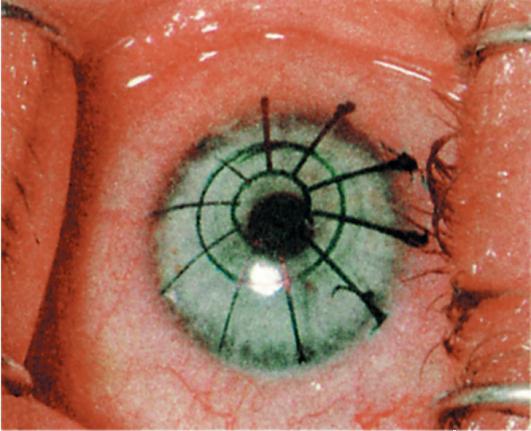
The markup before performing corneal incisions i>
This method is currently only of historical interest. Using corneal incision began in the late 19th century. Recent surgery myopia was established on the basis of ideas and experiments prof. Tsutomu Sato University of Tokyo (Tsutomu Sato of Juntendo University, Tokyo). He observed that the spontaneous rupture of Descemet membrane in keratoconus lead to a flattening of the cornea after healing. This was the basis for the formation of ideas about the rear corneal incision. He also noted that the damage to the eye from the Descemet's membrane is much more traumatic than the part of Bowman's membrane, but more effective. Later, in the 1940s, front cuts were introduced as an addition to the rear notch to amplify their effect after experimental study in rabbits tangensalnyh corneal incisions. Surgeons myopia patients began in Japan in the early 50s.
After the death of Sato and his followers surgery myopia in Japan slowed down and resumed in the USSR. Soviet ophthalmologists have come to the same conclusions. What and Sato. Front radial cuts were not as effective, they eventually came to the conclusion that the length and the distance from the limbus, and the depth of cut determine its effectiveness.
From 1970 to 1980, Fedorov and his colleagues have made a significant contribution to the development of the technique of radial keratotomy. Interest in technology operations led to the flow of American ophthalmologists Moskvu.V this time, he reported 99% satisfactory results of operations and he said that it has no more than 1-2 events per 1000 operations.
Subsequently it was found that the method has a significant complication in the case of eye injuries received after the correction. So, as the incisions for this method greatly disturbed architecture of the cornea, in the worst case after the injury occurred massive ruptures along the lines of cuts. "Collect" the cornea to normal after this was extremely difficult. The current method supplanted much safer and more physiologic LASIK / femto-LASIK.
Swifts lawn or how to get to the work area h4>

When I talk to employees about the differences between the variants LASIK and PRK, I call on the help of the following metaphor:
Imagine that you have a nice thick lawn. But, by a strange coincidence, just underneath is very necessary maintenance hatch, which you need to work. Lawn you want to keep in good form. You have two options:
Make a careful incision around the hatch and lift the turf. Under this option will be crossed by the roots and stems of the perimeter, but the grass is overgrown very quickly this seam. Grass on a raised turf will remain intact. trimmer to cut out and dig up the ground throughout the area over the hatch. Over time, the grass will grow again on the mowed area, but it will be much later. So, how many have already guessed, the grass symbolizes the corneal epithelium, and the two methods - LASIK / femto-LASIK and PRK, respectively. Accordingly, in embodiments, the flap is kept alive with the corneal epithelium, and the PRK option, although you can work with very thin corneas, but have a long recovery period for the regeneration of the epithelium.
PRK - photorefractive keratectomy h5>
In this method, a laser evaporation cornea occurs after removal of the upper fabric layer by chemical or mechanical means. This method does not provide for the creation of the flap-flap, which allows to use it in a very thin cornea. The method is fairly narrow application because of its difficult side effects and complications:
Potential corneal opacity - Hayes For the girls can not get pregnant within a year, use of hormonal contraceptives Long recovery period, often more than a month
LASIK - Laser-Assisted in Situ Keratomileusis h5>
The classical method which for many years. A distinctive feature - the removal flap apply special blade - microkeratome. Fixing microkeratome achieved by reducing the pressure zone. This method is more traumatic than its evolutionary continuation - femto-LASIK. Moreover conventional LASIK is banned in several countries, as of date, for example in Italy.
Femto-LASIK h5>
One of the most popular current methods, along with PRK. In contrast, KGF is stored in the integrity epithelium and Bowman's membrane. As a consequence, recovery time is minimized. Minimizes the risk of infection because they do not use power tools for forming the flap. It becomes possible to plan the individual profile of the flap, instead of the averaged form as in conventional LASIK. This makes it possible to design the optimal operation, as a result of providing quality vision.
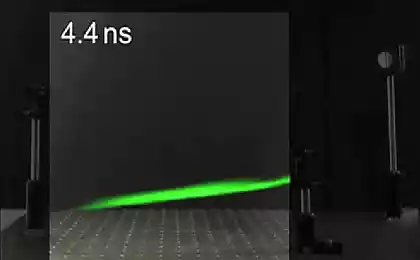
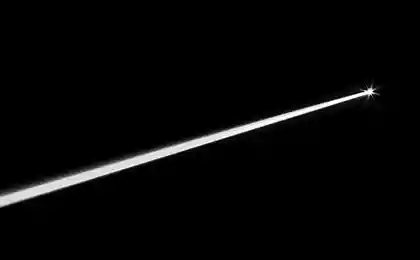
In order to form a flap, the first laser starts to form at a predetermined depth of cut. This is due to evaporation fabric under the beam. As a result of such exposure is formed, the gas bubble diameter of 2 microns. Distance between the individual bubbles 3 microns between turns of the spiral as the distance is 3 m. Energy per shot - 130-170 nJ on average. Accuracy of the highest. Individual parameters are adjusted depending on the specific situation and may vary within certain limits.
We are very proud of our excimer laser Amaris - primarily because of its safety and control systems of the set operation. In previous articles, many wondered what would happen if the patient twitches, the lights go out and the like. Consider the software and hardware implementation:
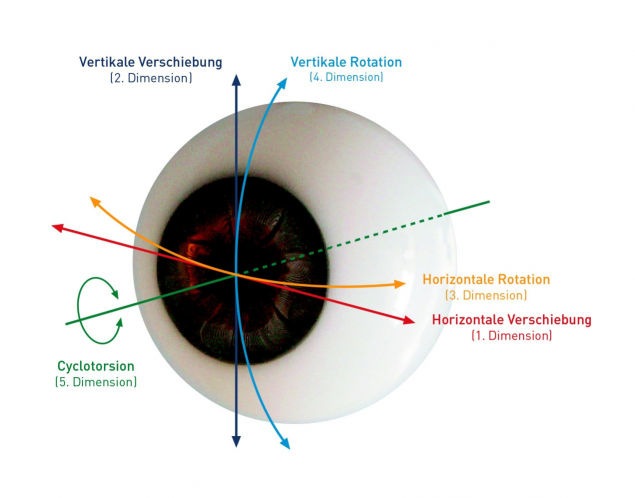
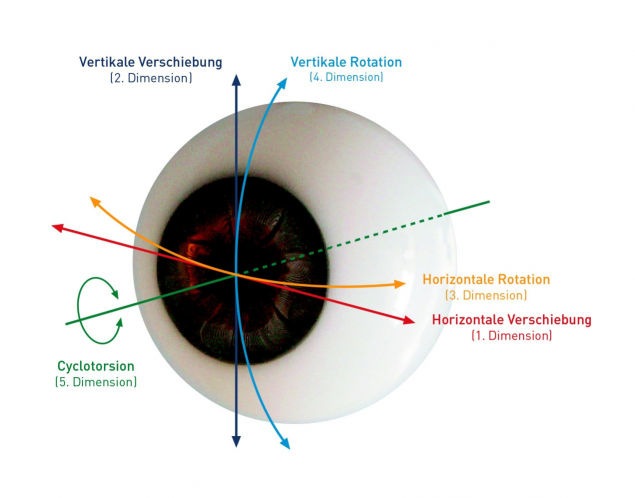
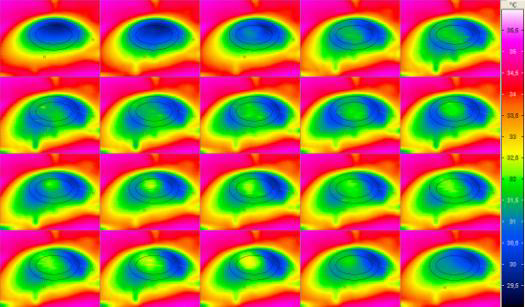
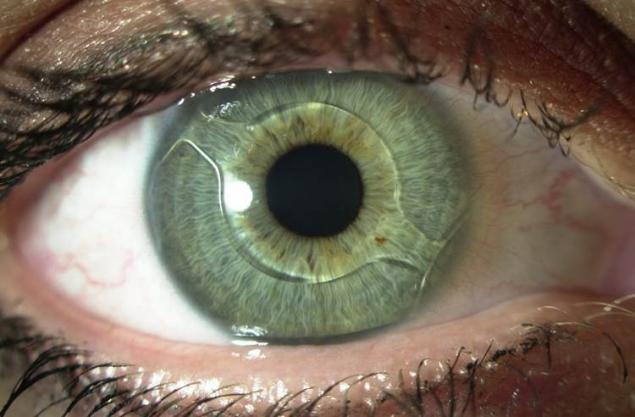
Eye movement control in five areas, including rotation. Before the operation there is a comparison picture of the iris and cornea evaporation given program. In the process of automatic controls and procedures specify the coordinates in which the laser works dynamically. The reaction time for the change in position of the working zone of not more than 3 ms. If the eye is too displaced relative to the operating position, the procedure is automatically terminated.
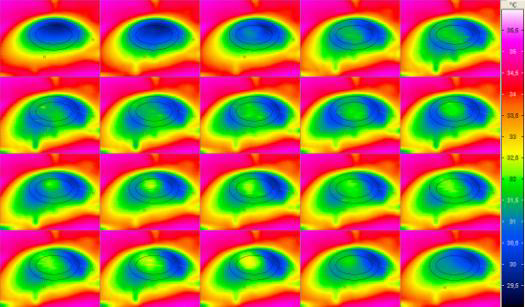
Special sensor continuously monitors the temperature of the surface of the cornea, preventing its damage due to overheating.
In the video you can see the system optimization power of the laser beam. Initially, the laser operates in the mode of high pulses that can quickly generate the desired curvature of the surface. The remaining 20% of the time the laser operates in the low-energy mode for a perfect surface smoothness. As a result, the system allows you to quickly and accurately remove a strictly predetermined amount of corneal tissue.
ReLEx Flex h5> < br />
Technology ReLEx Flex. The general principle is to scalloping of the flap with one femto laser. Then, after the tilt of the surface layer, the second flap is removed as a page from a book. As a result, the cornea changes shape as desired.
ReLEx Smile h5> < br />
Technology ReLEx Smile. Also runs a femto laser. The peculiarity of the method consists in cutting out the flap in lenticular thickness of the cornea, which is then gently removed with forceps through a small incision. As a result, the cornea is flattened in a predetermined manner and refraction bounces back.
Orthokeratology h5>

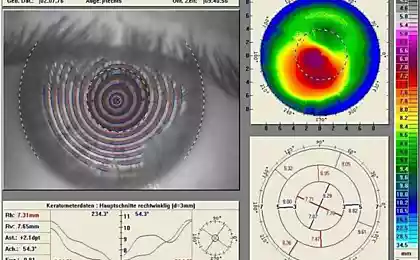
Orthokeratology - a technique which declares the refraction correction by wearing special hard contact lenses. The essence of the method in the progressive deformation of the cornea these lenses on a pre-designed pattern. I was repeatedly asked about the effectiveness and safety of this technique. After consulting with the collective intelligence of colleagues, we have come to a number of conclusions:
The technique is very young and there are no long-term results. Same LASIK with all its innovations like femto technology has long been studied for more than 20 years of observations. Methods supposedly aimed at cheapening the cost of correction and lowering the threshold entry into this business. For its application only and corneal topography machine vytachivaniya lenses. That is, once we save more than 40 million rubles for equipment operating modern lasers. Moreover, eliminating the need for full-profile clinic and an opportunity to work almost in the format of a pharmacy / optics in a small room. Naturally, it is attractive to many who promote this business model. Very doubtful duration of effect correction. When this method is stated reshaping cornea cells under the influence of hydraulic lens. However questionable long-term effects after a few years after the abolition of the impact of the lens Even normal lens wear is not useful for the cornea. Additional deforming effect can potentially lead to serious complications like keratitis, corneal epithelial disruption of the structure. Furthermore, mentioned about the dangers of wearing lenses at night, when the lid is closed, and oxygen to the cornea is supplied in a minimum amount. Hard contact lenses significantly worsen the situation and cause chronic corneal tissue anoxia.
After correction h4> Limiting visual loadings
After surgery, it is recommended to avoid excessive visual stress in the first few weeks. Eyes and brain need time to adapt to the new refraction. In fact uncommon for the patient is undergoing examination on Thursday, Friday operated, and on Monday did not take his eyes away from the monitor in the office. Of course, doctors do not approve of such, though the current pace of life dictates its conditions.
The limitation of physical activity
The first month after surgery is necessary to minimize the exercise, gradually come to the usual level by the end of this period. After months of physical rest, you can work out in the familiar rhythm as before. We must remember one very important thing - diagnosis myopia does not disappear after the correction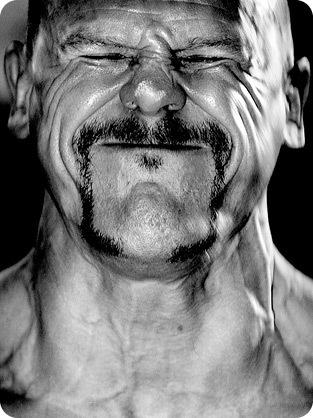

When there is no corneal h4>
The possible impact points i>
Unfortunately, there are situations when the cornea is too thin even for PRK, but for medical reasons a person really needs correction. For example, the large difference in diopters between the eyes can not give a person the opportunity to wear glasses. Most people without correction also can not manage. Then come to the aid of backup technologies, with their pros and cons. Naturally, these operations are shown not everyone.
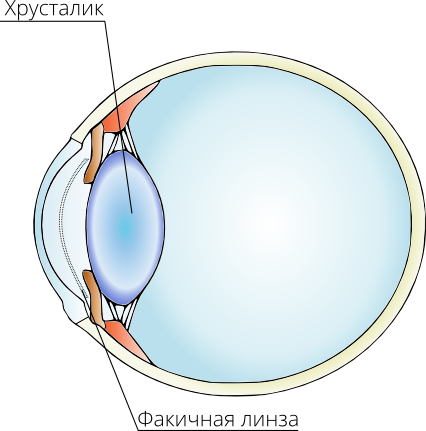
phakic lens h4>
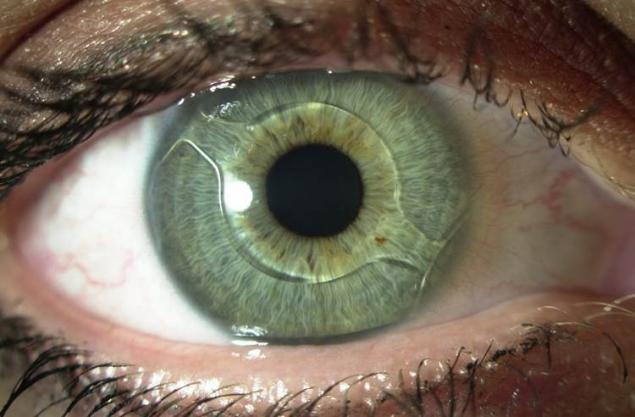
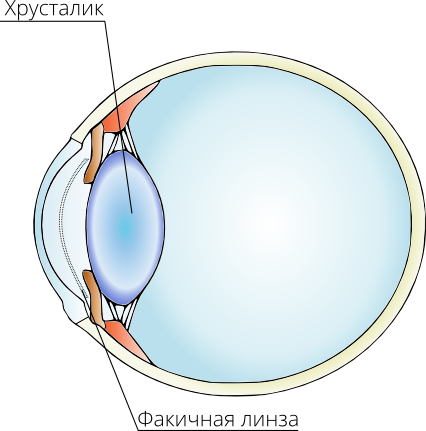
One option for the correction of refraction in a situation of very thin cornea is the use of phakic lenses. Clear lenses adjust the light beam to compensate for refractive errors. Usually applied at high myopia / hyperopia, when it is impossible due to the correction of refraction of the cornea. Have rather limited indications.
There are three types of phakic lenses which are implanted in order to correct refractive errors. Their name is determined by the location of the eyes: perednekamernaya phakic lens, iridofiksatsionnaya phakic lens (with fixation to the iris) and posterior chamber phakic lens.
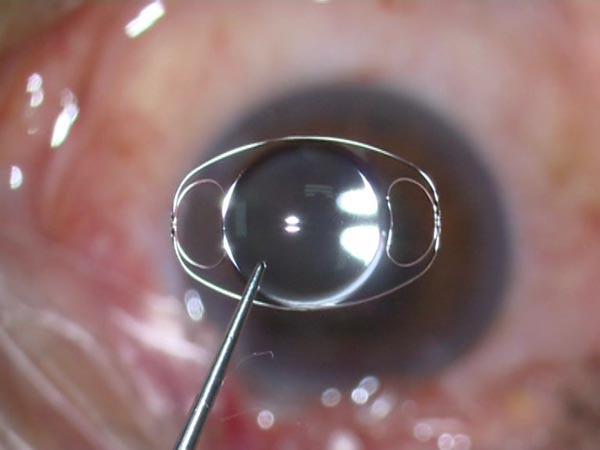
Appearance phakic lens i>
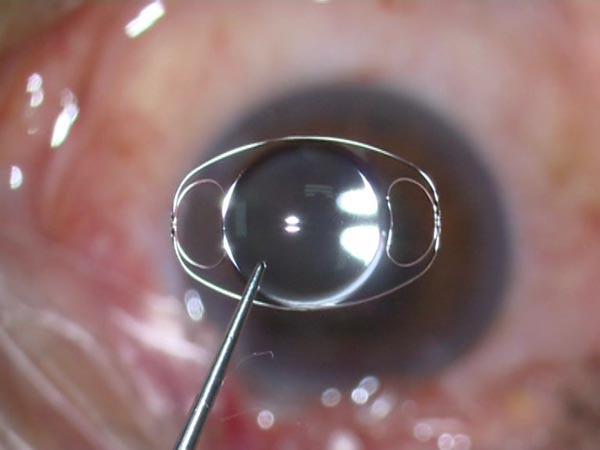
Replacement lens h4>

In the illustration, the doctor packs artificial lens in a special injector before implantation i>
This technique alone is worth a separate article.