1082
Oxalic acid and oxalates in food and in your body.
Oxalic acid is a substance that is part of some foods. It is an antinutrient that plants produce to protect against eating. In small amounts, it is harmless and is a byproduct of metabolism, which is easily excreted along with urine.
But high doses prevent the absorption of calcium and promote its accumulation. Sometimes, in a number of conditions, the normal excretion of salts of oxalic acid is disturbed. As a result, kidney and bladder stones, joint problems and systemic inflammation. Let's talk about it in more detail.
In principle, for a healthy person, the use of oxalates is safe. Scientists have established a safe amount of salts and esters of oxalic acid (oxalates) per 100 g of food in the amount of 50 mg. A healthy person can safely eat food with oxalates in moderation, but for people with kidney disease, gout, rheumatoid arthritis, it is recommended to avoid foods with large amounts of oxalates. Calcium oxalate crystals, better known as kidney stone, clog the kidney ducts. It is believed that 80% of kidney stones are formed from calcium oxalate.

The reasons for the increased content of oxalates, as well as the difficulties arising from their removal from the body, can be very different. The most banal is excessive abuse of fruits and vegetables, however, the probability of increasing the norm of oxalates from one food is extremely small. More often, oxalates in the urine occur in the form of sediment in pyelonephritis, during diseases for diabetes, or when poisoning with ethylene glycol. Common signs of oxaluria are severe fatigue, increased amount of urine during urination, pain in the stomach. From time to time, parents find in the general analysis of the urine of their children an increased content of calcium oxalate crystals. This is immediately alarming, because it is known that 75% of all kidney stones are calcium oxalates, and hyperoxaluria is characteristic of urolithiasis (ICD).
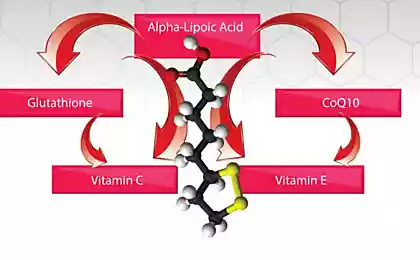
Mechanisms of harmful action of oxalatesOxaluria is the release in the urine of oxalate salts of oxalic acid in large quantities. The acid-base balance is disturbed in the direction of acidification of the environment - acidosis. The cause of acidosis may be the presence in the urine of calcium associated with oxalic acid, the acid itself and its crystals. In people with a violation of the exchange of oxalic acid per day, it is released about 1000 mg. At the same time, a person can feel unpleasant symptoms: pain in the side, lower abdomen, soreness during urination, the appearance of blood in the urine and many others. This is due to the irritating and traumatic effect of crystals on the mucous membrane of the urethra and other urinary organs. With such symptoms, you need to consult a doctor, pass all the necessary tests and undergo a full examination. You will also need to adjust the diet and, if necessary, take medications. Oxalic acid is not only formed in the body as a product of chemical reactions, it also comes from food. Consuming foods rich in it can lead to oxaluria and metabolic disorders of this substance. In the intestine, a small amount of this substance is also formed during the processing of carbohydrates by intestinal bacteria. Nerve excitation and overstrain stimulates the production of oxalic acid. Its concentration in the urine increases sharply, in medicine, this condition is called hyperoxaluria. In addition, oxalates and inflammation go hand in hand. Oxalates are oxidants, and oxidants create oxidative stress. In oxidative stress, molecules that should not be bound bind to each other.
Scientists have found that 40% of all oxalates are the result of chemical processes occurring in the liver, 20% is the result of metabolism of ascorbic acid, and 15% enters the body with food. An increase in the number of oxalates is associated with some diseases, such as obesity, liver disease and diabetes. Approximately 80 - 1200 mg of oxalate enters the body daily with food with normal nutrition, and if the diet is vegetarian - 80 - 2000 mg per day. About 10% of this oxalate is absorbed. In addition to intestinal absorption, oxalate is also formed endogenously, mainly from glyoxalic and ascorbic acids at a rate of about 1 mg / hour. Oxalate balance is achieved due to renal excretion - 15 - 40 mg / day. Oxalic acid serum can be divided into exogenous, which enters the body as a result of absorption from the gastrointestinal tract (30%), and endogenous, which is a product of metabolism (70%). Endogenous oxalate is formed in two ways:
Calcium oxalate crystals are excreted in the urine and have the characteristic shape of octahedrons ("mail envelopes") of different sizes. Crystals of another form are found, especially in cases where sprouts are formed. Their natural color is gray, but since they easily injure the mucous membrane, the blood pigment can stain them black. Oxalate crystals are found in acidic and alkaline urine.
There are primary (genetic) defects and secondary. Secondary disorders of oxalic acid metabolism arise due to exogenous (excessive intake of oxalogenous products, poor drinking regime, deficiency of magnesium, vitamins B2 and B6, the presence of diseases of the gastrointestinal tract) and other reasons:
1. The formation of crystals (calcium oxalates) in the urinary tract and other organs (lungs, joints, brain). Due to the specifics of the physical structure, such crystals can cause damage to the tissues of the body, accompanied by acute pain and the development of the inflammatory process.
2. The formation of complex compounds with heavy metals (mercury, lead, cadmium, etc.) is similar to the action of chelates. The task of detoxifying the body with the accumulation of problem oxalates is complicated. 3. The formation of oxalate salts with minerals such as calcium, magnesium, zinc, leads to a chronic shortage of these important trace elements in the body. The affinity of oxalate to divalent cations is reflected in the ability to form insoluble precipitation. So in the body, oxalate binds to cations such as Ca2+, Fe2+ and Mg2+. As a result, crystals of the corresponding oxalates accumulate, which, due to their shape, irritate the intestines and kidneys. Since oxalates bind important elements, such as calcium, long-term diets containing many oxalates can cause health problems.
In addition to kidney stones, a large amount of oxalic acid in the diet can cause other unpleasant symptoms, such as weakness, abdominal pain, indigestion, burning of the mucous membranes (oral cavity, throat and sinuses). In severe cases, it makes itself felt difficulty breathing and a violation of the cardiovascular system. About kidney stones are evidenced by severe pain from the back or abdominal cavity, as well as in the groin. Characteristic symptoms: Change in color of urine and pain when urinating. In some cases, nausea is possible. The main symptoms of oxaluria: abdominal pain, increased fatigue, frequent urination. How to determine the increase in oxalates? The complexes are deposited in the form of crystals, and the technician describes them in microscopy of urine sediment.
Where are the oxalates? The following list of foods includes the most common food sources of oxalates. It should be remembered that the leaves of plants contain more oxalates than in the roots or stems. Date and nut desserts and green smoothies can be wonderful, but they should not be consumed in large quantities every day.
Here are some high-oxalate foods. Rhubarb is one of the most generous plant sources of oxalic acid. It is present in all parts of the plant, but most of all in green leaves. Canned rhubarb contains 600 mg of oxalic acid for every 100 g, and unsweetened stew - up to 860 mg. Another source of oxalates. spinach. Frozen contains 600 mg per 100 g of green weight.
Among the natural sources of oxalic acid quite a lot of vegetables and fruits. For example, in 100g beet contains from 500 to 675 mg of this substance, chard - up to 645 mg, peels lemon and lime - from 83 to 110 mg, bami - 145 mg. Among medicinal herbs, the absolute favorite is lacquer - up to 475 mg. Fruit with oxalic acid: apples, raspberries and strawberries, gooseberry and blackberries, bananas, mangoes, black currants, pomegranates and oranges. Vegetables with oxalates: portulac and leaf mustard, potatoes and sweet potatoes, celery and asparagus, eggplant and pumpkin, beet top and radish, green and sweet pepper, chicory and tomatoes, parsnips, radishes and cauliflower, parsley and green onions. Beans, nuts and chocolate. Nuts, chocolate, legumes and some grains also have oxalic acid: 187 mg in fried peanuts, 202 mg in pecan nuts, 120 mg in classical chocolate, 270 mg in wheat germs. Dry cocoa powder contains an impressive 625 mg per 100 g. Other products with oxalic acid: amaranth, corn, wheat bran, oats, soybeans, beans and lentils. Lots of oxalates in buckwheat, almonds and cashews. Microflora and intestine Intestinal hyperoxaluria is often observed in patients with malabsorption syndrome, in which there is a violation of the processes of absorption of nutrients from the small intestine. This syndrome develops in various diseases of the gastrointestinal tract: inflammatory processes, enzyme insufficiency, disorders of motility and blood supply, dysbacteriosis, bypass anastomoses.
In a normal intestine, most oxalate binds to calcium and is excreted as insoluble compounds. The increase in the lumen of the intestine of non-absorbable fatty acids (steatorrhea) leads to the fact that they bind calcium and excreted in the form of calcium complexes. Thus, these patients do not have enough calcium to bind oxalate in the intestine and the absorption of oxalate increases. Decreased absorption of calcium causes hypocalcemia, which leads to secondary hyperparathyroidism and hypercalciuria - conditions are created for stone formation. Intestinal hyperoxaluria occurs as a result:
In recent years, there have been reports that a person in control of food oxalates helps one anaerobic bacteria, sheltered in our gastrointestinal tract on the rights of normal flora. Her name is Oxalobacter Formigenes. It is known that it eats only oxalates, it is its only source of energy, and that colonization of the intestines by Oxalobacter reduces the risk of stones and calcium oxalate by 70%. According to the hypothesis, if the content of O.formigenes in the gastrointestinal tract is reduced, then a greater amount of oxalates coming from food is absorbed in the intestine and enters the blood, and then into the urine, where crystals with calcium form. Studies have shown that most patients with oxalobacter formigenes are missing in the intestine. One potential reason for this is the use of antibiotics. For example, a 2-week eradication of Helicobacter pylori kills 63 percent of O.formigenes bacteria. And this violation of colonization persists for up to six months. Fat metabolism disorders. If you have a problem with bile and fat absorption, it will be optimal to limit the amount of fat. It's not about healthy people. To reduce the absorption of oxalates in intestinal pathology, it is recommended to limit the intake of fats, provide a diet with foods with a sufficient content of calcium and magnesium.
When consuming large amounts of fat with food, fatty acids bind calcium. This causes increased penetration of oxalic-acetic acid through the intestinal mucosa and increased its flow through the kidneys into the urine. Normally, oxalates contained in food bind to calcium in the intestinal lumen and are excreted from the body with feces in the form of insoluble calcium oxalate. Excessive absorption of oxalates in the intestine, which is associated with a violation of fat digestion, is the most common cause of oxalaturia (oxaluria). Therefore, with oxalaturia associated with pathology of the digestive organs, it is recommended to reduce fat intake to prevent increased absorption of oxalic acid salts.
In diseases of the digestive tract accompanied by malabsorption syndrome, fats that have not interacted with bile enzymes interact with calcium in the intestinal cavity forming soapy compounds, which is clinically manifested by steatorrhea. One of the protective actions of calcium is binding to an excess of intestinal lumen oxalates and elimination from the body in the form of oxalic acid calcium.
But, since most of the Ca went to interact with fats, the smaller binds oxalates, leading to their accumulation in the intestinal lumen in free form. At the same time, the lack of calcium leaves open intercellular spaces for the free penetration of excess oxalates into the bloodstream. Thus, we come to the conclusion that enteral restriction of calcium intake will not in any way affect the treatment of oxalate-calcium urolithiasis, but can even aggravate the state of the intestinal cell wall with the formation of the “leaky intestine” syndrome.
Magnesium deficiency.
Deficiency of protective colloids leads to insufficient intake of vitamins A, B, D and especially vitamin B6 and magnesium (studies of the causes of ICD confirm repeatedly that Ox in the urine are detected mainly in residents of areas with a natural deficiency of vitamin B6 and a lack of magnesium in drinking water and products). Vitamin B6 promotes the transition of glycocol to serine, which prevents the formation of aldehyde, from which oxalic acid (Ox) is formed in the human body by oxidation.
In the chemical reaction leading to the formation of crystals, only ionized forms of stone-forming substances take part. Thus, the amount of ionized calcium in the urine is 40-50%. Under normal conditions, the magnesium ion binds 30 to 40 percent of oxalates in the urine, competing with calcium. Due to the chemical antagonism of calcium and magnesium, additional magnesium intake reduces the formation of calcium oxalate. Experimental, epidemiological and clinical evidence suggests that a lack of magnesium in food can contribute to the formation of oxalates, and the enrichment of the diet with magnesium contributes to the excretion of oxalates.
Other tips to reduce the level of oxalates.
1. Boiling (with water draining). Green leafy vegetables should be held a little in boiling water before cooking (water drain) - this reduces the level of oxalates. Heat treatment with water drainage, cooking in two waters. Use fresh, young leaves.
2. Add calcium-rich foods. There are enough foods that contain calcium. When the amount of calcium and the amount of oxalates in food is balanced, the crystals are formed in the intestine, and are not absorbed into the blood. If the balance is disturbed in favor of oxalates, the formation of crystals occurs already in the kidneys and urinary system. Large intakes of calcium together with food containing oxalates leads to the loss of calcium oxalate in the digestive tract, reducing the intake of oxalates in the body by 97%.
3. Drink enough water, well - mineral water.
4. Use of citrates. Add lemon juice to drinks (100 grams per day, distribute for each drink). Often, the urologist prescribes sodium citrate and potassium citrate to the patient, thereby reducing the formation of complexes of insoluble calcium salts, reducing the concentration of its ions and forming complexes with citrate. D.
5. Stop taking complexes with vitamin C. An excess of vitamin C increases the amount of oxalic acid. An increase in the production of oxalates in the body also causes excessive consumption of ascorbic acid, which is metabolized in the body into oxalic acid.
Conclusion. Increasing the level of oxalic acid and oxalates is an important basis for the development of a number of diseases. A low-oxalate diet can help a lot.
Annex The oxalate table below is based on data from the most up-to-date sources. Possible discrepancies with those in earlier sources are explained by the use of improved precision methods for measuring oxalic acid salts and/or by different types (varieties) of a product in different geographical areas.
For the convenience of diet planning, all products are distributed into three groups:
Group 1 - products containing a low amount of oxalates (less than 2 mg per 1 serving). There is no need to restrict such products.
Group 2 - products containing an average amount of oxalates (2 to 6 mg per serving). It should be limited to three portions of such products per day.
3 Group - products with a high content of oxalates (more than 7 mg per serving). Such products should be excluded from the diet.
* The icon indicates products that are exceptionally high in oxalates (50 to 700 mg) per serving.
1 serving is:
lemonade milk wine water Coca-Cola teas herbal apple juice orange juice
grape juice
cranberry juice coffee carrot juice tomato juice tea green Any juice made from highly oxalate fruits
Cocoa beer chocolate chocolate chocolate milk coffee instant tea black tea rosehip tea Vegetables Low oxalate density Average oxalate density High oxalate density Fungi
green peas cabbage chestnuts kohlrabi cucumbers pepper red radish pumpkin cauliflower shnitt onions Artichoke
broccoli Brussels sprout peas canned sauerkraut corn cress salad turnip onions (roots) lettuce asparagus tomato paste eggplant
green leafy vegetables* potatoes kale leeks* carrots dandelion okra* peppers green and chilli parsley (greens) beets (and tips and roots)* celery pumpkin summer yellow beans (and pod and dry) zucchini spinach* sorrel yams (bath) Fruit Low oxalate density Average oxalate density High oxalate density avocado
watermelon banana (small) grapes green melon cranberry nectarines blueberry apples peeled apricots
pineapple banana grapes dark cherry pear grapefruit raisins cranberry dried strawberry coconut lemon mandarin
papaya
peaches plum currant black cherries prunes apples with orange skin (more than 1/2)
Grapes dark blackberries figs kiwi gooseberry raspberries red dates persimmon peel orange lime peel lemon* Nuts, seeds, beans and legumes Low oxalate density Average oxalate density High oxalate density Chestnuts Boiled dry peas
chickpeas flax seed pumpkin beans lima lentils red (30 minutes of cooking) Peanuts*
peanut butter* walnuts cedar nuts cashew sesame* and its oil poppy* almonds* pecans* sunflower seeds* chia soybeans* tofu* pistachios* hazelnuts* lentils Cereals and products from them, substitutes for baking
Low oxalate density Average oxalate density High oxalate density Tapioka starch Coconut flour Pumpkin seed flour Pasta products Rice (white and wild) and products from it Rice flour Bread Morning breakfast cereals (cereals) Starch
corn bread corn cakes flour (wheat) oatmeal barley rice brown and products from it spaghetti with tomato sauce buckwheat*
Wheat germ * kamut kinwa (quinoa) * corn cereal marmalade millet rye soy flour * teff * rye and wheat breads Meat, fish, bird
Low oxalate density Average oxalate density High oxalate density Lamb beef poultry seafood fish pork eggs Beef kidney liver sardines No Dairy products
Low oxalate density Average oxalate density High oxalate density Yogurt milk (natural without additives or with allowed fruits) Chocolate milk Fats and oils have a low oxalate density (except sesame oil). Different. Low oxalate density Average oxalate density High oxalate density Gelatin carob ketchup (1 tbsp) maple syrup honey sugar agave spirulina dill syrup (up to 1 tsp) vinegar All spices that are not listed on the right, including (mustard (up to 1 tbsp), garlic, extracts: lemon, ginger, crystallized ginger, paprika sweet, fresh cilantro, fresh basil (1 tsp) raw ginger white pepper) Tobazier sauce P (1st tbsp.), garlic with a small potato in 1 drizzle. And remember, just changing our consumption – together we change the world!
Join us on Facebook, VKontakte, Odnoklassniki
Source: www.beloveshkin.com/2015/08/shhavelevaya-kislota-i-oksalaty-v-produktakh-pitaniya-i-v-vashem-tele.html
But high doses prevent the absorption of calcium and promote its accumulation. Sometimes, in a number of conditions, the normal excretion of salts of oxalic acid is disturbed. As a result, kidney and bladder stones, joint problems and systemic inflammation. Let's talk about it in more detail.
In principle, for a healthy person, the use of oxalates is safe. Scientists have established a safe amount of salts and esters of oxalic acid (oxalates) per 100 g of food in the amount of 50 mg. A healthy person can safely eat food with oxalates in moderation, but for people with kidney disease, gout, rheumatoid arthritis, it is recommended to avoid foods with large amounts of oxalates. Calcium oxalate crystals, better known as kidney stone, clog the kidney ducts. It is believed that 80% of kidney stones are formed from calcium oxalate.

The reasons for the increased content of oxalates, as well as the difficulties arising from their removal from the body, can be very different. The most banal is excessive abuse of fruits and vegetables, however, the probability of increasing the norm of oxalates from one food is extremely small. More often, oxalates in the urine occur in the form of sediment in pyelonephritis, during diseases for diabetes, or when poisoning with ethylene glycol. Common signs of oxaluria are severe fatigue, increased amount of urine during urination, pain in the stomach. From time to time, parents find in the general analysis of the urine of their children an increased content of calcium oxalate crystals. This is immediately alarming, because it is known that 75% of all kidney stones are calcium oxalates, and hyperoxaluria is characteristic of urolithiasis (ICD).
Mechanisms of harmful action of oxalatesOxaluria is the release in the urine of oxalate salts of oxalic acid in large quantities. The acid-base balance is disturbed in the direction of acidification of the environment - acidosis. The cause of acidosis may be the presence in the urine of calcium associated with oxalic acid, the acid itself and its crystals. In people with a violation of the exchange of oxalic acid per day, it is released about 1000 mg. At the same time, a person can feel unpleasant symptoms: pain in the side, lower abdomen, soreness during urination, the appearance of blood in the urine and many others. This is due to the irritating and traumatic effect of crystals on the mucous membrane of the urethra and other urinary organs. With such symptoms, you need to consult a doctor, pass all the necessary tests and undergo a full examination. You will also need to adjust the diet and, if necessary, take medications. Oxalic acid is not only formed in the body as a product of chemical reactions, it also comes from food. Consuming foods rich in it can lead to oxaluria and metabolic disorders of this substance. In the intestine, a small amount of this substance is also formed during the processing of carbohydrates by intestinal bacteria. Nerve excitation and overstrain stimulates the production of oxalic acid. Its concentration in the urine increases sharply, in medicine, this condition is called hyperoxaluria. In addition, oxalates and inflammation go hand in hand. Oxalates are oxidants, and oxidants create oxidative stress. In oxidative stress, molecules that should not be bound bind to each other.
Scientists have found that 40% of all oxalates are the result of chemical processes occurring in the liver, 20% is the result of metabolism of ascorbic acid, and 15% enters the body with food. An increase in the number of oxalates is associated with some diseases, such as obesity, liver disease and diabetes. Approximately 80 - 1200 mg of oxalate enters the body daily with food with normal nutrition, and if the diet is vegetarian - 80 - 2000 mg per day. About 10% of this oxalate is absorbed. In addition to intestinal absorption, oxalate is also formed endogenously, mainly from glyoxalic and ascorbic acids at a rate of about 1 mg / hour. Oxalate balance is achieved due to renal excretion - 15 - 40 mg / day. Oxalic acid serum can be divided into exogenous, which enters the body as a result of absorption from the gastrointestinal tract (30%), and endogenous, which is a product of metabolism (70%). Endogenous oxalate is formed in two ways:
- As a result of metabolism of ascorbic acid (30%).
- As a result of glyoxalic acid metabolism (40%).
Calcium oxalate crystals are excreted in the urine and have the characteristic shape of octahedrons ("mail envelopes") of different sizes. Crystals of another form are found, especially in cases where sprouts are formed. Their natural color is gray, but since they easily injure the mucous membrane, the blood pigment can stain them black. Oxalate crystals are found in acidic and alkaline urine.
There are primary (genetic) defects and secondary. Secondary disorders of oxalic acid metabolism arise due to exogenous (excessive intake of oxalogenous products, poor drinking regime, deficiency of magnesium, vitamins B2 and B6, the presence of diseases of the gastrointestinal tract) and other reasons:
1. The formation of crystals (calcium oxalates) in the urinary tract and other organs (lungs, joints, brain). Due to the specifics of the physical structure, such crystals can cause damage to the tissues of the body, accompanied by acute pain and the development of the inflammatory process.
2. The formation of complex compounds with heavy metals (mercury, lead, cadmium, etc.) is similar to the action of chelates. The task of detoxifying the body with the accumulation of problem oxalates is complicated. 3. The formation of oxalate salts with minerals such as calcium, magnesium, zinc, leads to a chronic shortage of these important trace elements in the body. The affinity of oxalate to divalent cations is reflected in the ability to form insoluble precipitation. So in the body, oxalate binds to cations such as Ca2+, Fe2+ and Mg2+. As a result, crystals of the corresponding oxalates accumulate, which, due to their shape, irritate the intestines and kidneys. Since oxalates bind important elements, such as calcium, long-term diets containing many oxalates can cause health problems.
In addition to kidney stones, a large amount of oxalic acid in the diet can cause other unpleasant symptoms, such as weakness, abdominal pain, indigestion, burning of the mucous membranes (oral cavity, throat and sinuses). In severe cases, it makes itself felt difficulty breathing and a violation of the cardiovascular system. About kidney stones are evidenced by severe pain from the back or abdominal cavity, as well as in the groin. Characteristic symptoms: Change in color of urine and pain when urinating. In some cases, nausea is possible. The main symptoms of oxaluria: abdominal pain, increased fatigue, frequent urination. How to determine the increase in oxalates? The complexes are deposited in the form of crystals, and the technician describes them in microscopy of urine sediment.
Where are the oxalates? The following list of foods includes the most common food sources of oxalates. It should be remembered that the leaves of plants contain more oxalates than in the roots or stems. Date and nut desserts and green smoothies can be wonderful, but they should not be consumed in large quantities every day.
- large (> 1 g / kg) amount is contained in cocoa beans, chocolate, celery, spinach, sorrel, parsley, rhubarb;
- moderate (0.3 - 1.0 g / kg) - in carrots, beets, chicory, green beans, onions, tomatoes, tea;
- small (0.05 - 0.3 g / kg) amount - in fresh cabbage, apricots, bananas, currants, Brussels sprouts, potatoes;
- The least amount of oxalic acid contains eggplant, cucumbers, pumpkin, mushrooms, cauliflower, lettuce leaves, peas.
Here are some high-oxalate foods. Rhubarb is one of the most generous plant sources of oxalic acid. It is present in all parts of the plant, but most of all in green leaves. Canned rhubarb contains 600 mg of oxalic acid for every 100 g, and unsweetened stew - up to 860 mg. Another source of oxalates. spinach. Frozen contains 600 mg per 100 g of green weight.
Among the natural sources of oxalic acid quite a lot of vegetables and fruits. For example, in 100g beet contains from 500 to 675 mg of this substance, chard - up to 645 mg, peels lemon and lime - from 83 to 110 mg, bami - 145 mg. Among medicinal herbs, the absolute favorite is lacquer - up to 475 mg. Fruit with oxalic acid: apples, raspberries and strawberries, gooseberry and blackberries, bananas, mangoes, black currants, pomegranates and oranges. Vegetables with oxalates: portulac and leaf mustard, potatoes and sweet potatoes, celery and asparagus, eggplant and pumpkin, beet top and radish, green and sweet pepper, chicory and tomatoes, parsnips, radishes and cauliflower, parsley and green onions. Beans, nuts and chocolate. Nuts, chocolate, legumes and some grains also have oxalic acid: 187 mg in fried peanuts, 202 mg in pecan nuts, 120 mg in classical chocolate, 270 mg in wheat germs. Dry cocoa powder contains an impressive 625 mg per 100 g. Other products with oxalic acid: amaranth, corn, wheat bran, oats, soybeans, beans and lentils. Lots of oxalates in buckwheat, almonds and cashews. Microflora and intestine Intestinal hyperoxaluria is often observed in patients with malabsorption syndrome, in which there is a violation of the processes of absorption of nutrients from the small intestine. This syndrome develops in various diseases of the gastrointestinal tract: inflammatory processes, enzyme insufficiency, disorders of motility and blood supply, dysbacteriosis, bypass anastomoses.
In a normal intestine, most oxalate binds to calcium and is excreted as insoluble compounds. The increase in the lumen of the intestine of non-absorbable fatty acids (steatorrhea) leads to the fact that they bind calcium and excreted in the form of calcium complexes. Thus, these patients do not have enough calcium to bind oxalate in the intestine and the absorption of oxalate increases. Decreased absorption of calcium causes hypocalcemia, which leads to secondary hyperparathyroidism and hypercalciuria - conditions are created for stone formation. Intestinal hyperoxaluria occurs as a result:
- insufficient formation of calcium oxalate complexes in the intestine as a result of low calcium content due to a decrease in calcium intake with food or the formation of calcium + fatty acid complexes in patients with gastrointestinal disorders;
- increased absorption of oxalic acid for unknown reasons;
- use of very high doses of ascorbic acid;
- Decreased population of bacteria Oxalobacter formigenes.
In recent years, there have been reports that a person in control of food oxalates helps one anaerobic bacteria, sheltered in our gastrointestinal tract on the rights of normal flora. Her name is Oxalobacter Formigenes. It is known that it eats only oxalates, it is its only source of energy, and that colonization of the intestines by Oxalobacter reduces the risk of stones and calcium oxalate by 70%. According to the hypothesis, if the content of O.formigenes in the gastrointestinal tract is reduced, then a greater amount of oxalates coming from food is absorbed in the intestine and enters the blood, and then into the urine, where crystals with calcium form. Studies have shown that most patients with oxalobacter formigenes are missing in the intestine. One potential reason for this is the use of antibiotics. For example, a 2-week eradication of Helicobacter pylori kills 63 percent of O.formigenes bacteria. And this violation of colonization persists for up to six months. Fat metabolism disorders. If you have a problem with bile and fat absorption, it will be optimal to limit the amount of fat. It's not about healthy people. To reduce the absorption of oxalates in intestinal pathology, it is recommended to limit the intake of fats, provide a diet with foods with a sufficient content of calcium and magnesium.
When consuming large amounts of fat with food, fatty acids bind calcium. This causes increased penetration of oxalic-acetic acid through the intestinal mucosa and increased its flow through the kidneys into the urine. Normally, oxalates contained in food bind to calcium in the intestinal lumen and are excreted from the body with feces in the form of insoluble calcium oxalate. Excessive absorption of oxalates in the intestine, which is associated with a violation of fat digestion, is the most common cause of oxalaturia (oxaluria). Therefore, with oxalaturia associated with pathology of the digestive organs, it is recommended to reduce fat intake to prevent increased absorption of oxalic acid salts.
In diseases of the digestive tract accompanied by malabsorption syndrome, fats that have not interacted with bile enzymes interact with calcium in the intestinal cavity forming soapy compounds, which is clinically manifested by steatorrhea. One of the protective actions of calcium is binding to an excess of intestinal lumen oxalates and elimination from the body in the form of oxalic acid calcium.
But, since most of the Ca went to interact with fats, the smaller binds oxalates, leading to their accumulation in the intestinal lumen in free form. At the same time, the lack of calcium leaves open intercellular spaces for the free penetration of excess oxalates into the bloodstream. Thus, we come to the conclusion that enteral restriction of calcium intake will not in any way affect the treatment of oxalate-calcium urolithiasis, but can even aggravate the state of the intestinal cell wall with the formation of the “leaky intestine” syndrome.
Magnesium deficiency.
Deficiency of protective colloids leads to insufficient intake of vitamins A, B, D and especially vitamin B6 and magnesium (studies of the causes of ICD confirm repeatedly that Ox in the urine are detected mainly in residents of areas with a natural deficiency of vitamin B6 and a lack of magnesium in drinking water and products). Vitamin B6 promotes the transition of glycocol to serine, which prevents the formation of aldehyde, from which oxalic acid (Ox) is formed in the human body by oxidation.
In the chemical reaction leading to the formation of crystals, only ionized forms of stone-forming substances take part. Thus, the amount of ionized calcium in the urine is 40-50%. Under normal conditions, the magnesium ion binds 30 to 40 percent of oxalates in the urine, competing with calcium. Due to the chemical antagonism of calcium and magnesium, additional magnesium intake reduces the formation of calcium oxalate. Experimental, epidemiological and clinical evidence suggests that a lack of magnesium in food can contribute to the formation of oxalates, and the enrichment of the diet with magnesium contributes to the excretion of oxalates.
Other tips to reduce the level of oxalates.
1. Boiling (with water draining). Green leafy vegetables should be held a little in boiling water before cooking (water drain) - this reduces the level of oxalates. Heat treatment with water drainage, cooking in two waters. Use fresh, young leaves.
2. Add calcium-rich foods. There are enough foods that contain calcium. When the amount of calcium and the amount of oxalates in food is balanced, the crystals are formed in the intestine, and are not absorbed into the blood. If the balance is disturbed in favor of oxalates, the formation of crystals occurs already in the kidneys and urinary system. Large intakes of calcium together with food containing oxalates leads to the loss of calcium oxalate in the digestive tract, reducing the intake of oxalates in the body by 97%.
3. Drink enough water, well - mineral water.
4. Use of citrates. Add lemon juice to drinks (100 grams per day, distribute for each drink). Often, the urologist prescribes sodium citrate and potassium citrate to the patient, thereby reducing the formation of complexes of insoluble calcium salts, reducing the concentration of its ions and forming complexes with citrate. D.
5. Stop taking complexes with vitamin C. An excess of vitamin C increases the amount of oxalic acid. An increase in the production of oxalates in the body also causes excessive consumption of ascorbic acid, which is metabolized in the body into oxalic acid.
Conclusion. Increasing the level of oxalic acid and oxalates is an important basis for the development of a number of diseases. A low-oxalate diet can help a lot.
Annex The oxalate table below is based on data from the most up-to-date sources. Possible discrepancies with those in earlier sources are explained by the use of improved precision methods for measuring oxalic acid salts and/or by different types (varieties) of a product in different geographical areas.
For the convenience of diet planning, all products are distributed into three groups:
Group 1 - products containing a low amount of oxalates (less than 2 mg per 1 serving). There is no need to restrict such products.
Group 2 - products containing an average amount of oxalates (2 to 6 mg per serving). It should be limited to three portions of such products per day.
3 Group - products with a high content of oxalates (more than 7 mg per serving). Such products should be excluded from the diet.
* The icon indicates products that are exceptionally high in oxalates (50 to 700 mg) per serving.
1 serving is:
- 1/2 cup juice, berries
- 1 small fruit
- 1⁄4 cup of dried fruit
- 1 cup of fresh salad greens
- 1⁄2 cup of cut vegetables (in raw or boiled form)
- 2 tbsp nuts and seeds
- about 30g cheese
- 1 cup of milk or its substitutes
- half a glass of cereal or pasta finished
- 1 piece of bread
lemonade milk wine water Coca-Cola teas herbal apple juice orange juice
grape juice
cranberry juice coffee carrot juice tomato juice tea green Any juice made from highly oxalate fruits
Cocoa beer chocolate chocolate chocolate milk coffee instant tea black tea rosehip tea Vegetables Low oxalate density Average oxalate density High oxalate density Fungi
green peas cabbage chestnuts kohlrabi cucumbers pepper red radish pumpkin cauliflower shnitt onions Artichoke
broccoli Brussels sprout peas canned sauerkraut corn cress salad turnip onions (roots) lettuce asparagus tomato paste eggplant
green leafy vegetables* potatoes kale leeks* carrots dandelion okra* peppers green and chilli parsley (greens) beets (and tips and roots)* celery pumpkin summer yellow beans (and pod and dry) zucchini spinach* sorrel yams (bath) Fruit Low oxalate density Average oxalate density High oxalate density avocado
watermelon banana (small) grapes green melon cranberry nectarines blueberry apples peeled apricots
pineapple banana grapes dark cherry pear grapefruit raisins cranberry dried strawberry coconut lemon mandarin
papaya
peaches plum currant black cherries prunes apples with orange skin (more than 1/2)
Grapes dark blackberries figs kiwi gooseberry raspberries red dates persimmon peel orange lime peel lemon* Nuts, seeds, beans and legumes Low oxalate density Average oxalate density High oxalate density Chestnuts Boiled dry peas
chickpeas flax seed pumpkin beans lima lentils red (30 minutes of cooking) Peanuts*
peanut butter* walnuts cedar nuts cashew sesame* and its oil poppy* almonds* pecans* sunflower seeds* chia soybeans* tofu* pistachios* hazelnuts* lentils Cereals and products from them, substitutes for baking
Low oxalate density Average oxalate density High oxalate density Tapioka starch Coconut flour Pumpkin seed flour Pasta products Rice (white and wild) and products from it Rice flour Bread Morning breakfast cereals (cereals) Starch
corn bread corn cakes flour (wheat) oatmeal barley rice brown and products from it spaghetti with tomato sauce buckwheat*
Wheat germ * kamut kinwa (quinoa) * corn cereal marmalade millet rye soy flour * teff * rye and wheat breads Meat, fish, bird
Low oxalate density Average oxalate density High oxalate density Lamb beef poultry seafood fish pork eggs Beef kidney liver sardines No Dairy products
Low oxalate density Average oxalate density High oxalate density Yogurt milk (natural without additives or with allowed fruits) Chocolate milk Fats and oils have a low oxalate density (except sesame oil). Different. Low oxalate density Average oxalate density High oxalate density Gelatin carob ketchup (1 tbsp) maple syrup honey sugar agave spirulina dill syrup (up to 1 tsp) vinegar All spices that are not listed on the right, including (mustard (up to 1 tbsp), garlic, extracts: lemon, ginger, crystallized ginger, paprika sweet, fresh cilantro, fresh basil (1 tsp) raw ginger white pepper) Tobazier sauce P (1st tbsp.), garlic with a small potato in 1 drizzle. And remember, just changing our consumption – together we change the world!
Join us on Facebook, VKontakte, Odnoklassniki
Source: www.beloveshkin.com/2015/08/shhavelevaya-kislota-i-oksalaty-v-produktakh-pitaniya-i-v-vashem-tele.html