879
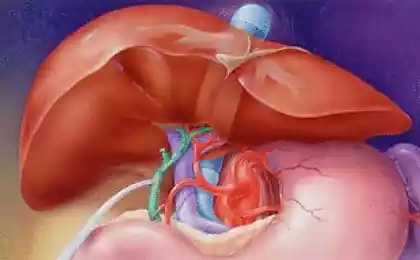
Leptinresistance and fatty liver disease
It all starts with the liver: leptinresistance and fat disease.
Almost every third person (according to others – every second!) found changes in the liver (fatty liver disease). Today we learn that resistance to the leptin begins with changes in the liver. And learn how dangerous fat in the liver, how it's measured and what it says.
To understand the relationship of stress, our reaction to it, it is important to know that stress is almost always associated with the accumulation of "bad" fat (the internal fat, visceral or abdominal fat). "Bad fat," causes inflammation, which increases stress and everything moves in a circle.
This mode of deficit, which manifests itself in all areas of human life: in mood, motivation, energy levels, appearance, activity, weight, disease, the psyche, and even in relationships with other people. As the proverb says, "with fat rage".But the "bad fat" is not always associated with excess weight. In addition, there are "good" fat, which is a great source of energy.
Forty five million two hundred four thousand three hundred eleven
Therefore, I will examine a number of cases in a not so obvious "bad" fat. Is fatty liver disease, skinny people with internal obesity and people of normal weight who are "fat inside". For balance, I will write about fat people who are healthy and not fat. Unfortunately, these nuances of the few who does, but they are critical to health. You consider yourself lean and not fat? Then we go to you! A more precisely, to your liver!
Fatty liver (fatty liver disease) is the Rubicon, which overeating and drinking turns into a real disease. The accumulation of fat in the liver called non-alcoholic fatty liver disease (NAFLD). I must say that there are alcoholic fatty liver disease, which is not much different (except for cause).
Have NAFLD, there are the following variants of the course:
steatosis (type 1) — the predominance of fatty degeneration of hepatocytes over all other morphological changes,
steatohepatitis (type 2) is expressed by inflammatory infiltrates in the stroma and the parenchyma with the presence of focal necrosis,
statefips (type 3) — predominance of fibrosis of the portal stroma, but without disruption of lobular structure, steatosis — a violation of the lobular structure of the liver with the presence of nodes regenerates. NAFLD can be a manifestation of various diseases and pathology
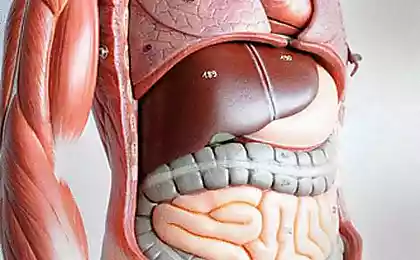
Nonalcoholic hepatic steatosis (nonalcoholic fatty liver disease (NAFLD), fatty liver, fatty liver, fatty infiltration) — primary liver disease or a syndrome generated by excess accumulation of fat (mainly triglycerides) in the liver. Normal liver contains about 5% fat. If we consider this nosology from a quantitative point of view, "fat" should be at least 5-10% of liver weight, or more than 5% of hepatocytes should contain lipids (histologically). It's a little! Ie, the disease is already active flows, if the fat has accumulated more than 5% of liver cells! Please note this fact!
Twenty four million seven hundred nine thousand four hundred seventy three
The course and manifestations of fatty liver disease.
1. Can occur bessimptomnom, found by accident.In many patients the liver detected by chance during examinations for other diseases.
2.Has mild symptoms.The disease is typically of long duration with minimal or moderate inflammation activity in the liver. In most patients, symptoms characteristic of liver disease are absent. Sometimes there are complaints of heaviness and discomfort in the right upper quadrant of the abdomen, aggravated by movement, fatigue, weakness, nausea. Often the disease is diagnosed accidentally during ultrasound examination of the liver after its enlargement and hyperechogenicity or "brightness" of the liver tissue due to diffuse fatty infiltration.
3. If you have normal tests, it does not exclude problems with the liver! Elevated levels of serum transaminases revealed only 20-21% of patients with NAFLD. However, normal levels of transaminases do not exclude veroyatnostnaya necrotic-inflammatory changes and fibrosis of the liver.
3. Happens in people with normal body weight. The increase in its incidence parallel to the obesity epidemic has allowed for the confirmation of fatty liver disease to use the body mass index (BMI). At the same time up to 25 % of patients with NAFLD may not be obese but have a clear laboratory evidence of IR.
4. Very slowly progressing. Usually steatosis is characterized by stable, non-progressive course. If to fatty infiltration joins the inflammatory process, that is developed steatohepatitis, the disease often progresses with the formation of liver fibrosis (30-40% of patients) and cirrhosis (approximately 10 %).
5. Fatty liver disease totally reversible! About this will be later. It should be noted the possibility of reverse development of nonalcoholic fatty disease on the background of reducing weight (and / or visceral fat).
6. Fatty liver disease is very common.The prevalence of non-alcoholic hepatic steatosis among residents of economically developed countries is an average of 2035%, non-alcoholic steatohepatitis and 3% [21, 29]. In the US hepatic steatosis have 34% of the adult population in Japan – 29% [10, 36]. In Russia, according to a screening program to identify the prevalence of NAFLD and its clinical forms, carried out in 2007 and engulfed 30754 people, NAFLD was diagnosed in 27% of patients.
7. Obesity is a problem with the liver is almost always.In obese patients the prevalence of different clinical forms of NAFLD are significantly higher than in the General population, and is, according to studies, up to 93%. According to Tarantino G. et al. (2007), steatosis is diagnosed in 10-25% of the U.S. population, including in 57-75% of patients with morbid (body mass index >30-35) obese and nearly 100% of with obesity and type 2 diabetes. It is noted feedback: patients with NAFLD revealed obesity in 30-100% of cases, type 2 diabetes in 10 to 75%, hyperlipidemia in 20-92% of cases.
Sixty three million nine hundred one thousand four
How is fatty liver disease? For the development of fatty disease need two strokes. The first shot is poor nutrition. When the fat accumulates in the liver. The second blow is inflammation and oxidation (oxidative stress). Fat is oxidized and becomes "bad" fat, i.e., produces compounds that trigger inflammation.
Blow to the liver can be applied not only fast food but also alcohol. Alcoholic fatty liver disease like non-alcoholic, and the result is the same! Traced a direct correlation of the type of liver disease the dose of alcohol consumed daily.
It should be noted that the type of drink is not important, important is the amount of alcohol. It was noted that alcohol is the main cause of liver disease in Europe. Perhaps a combination of alcoholic liver disease and NAFLD. Fatty degeneration of the liver occurs more frequently in individuals with obesity, history of alcohol abuse. Safe dose of alcohol that do not cause the progression of NAFLD has not been established.
Forty three million twenty five thousand five hundred ninety eight
The first blow (fat accumulates) When people eat a meal, about 60% of the calories is deposited in the liver to provide the tissues with energy in between meals. Another hormone, glucagon, mediates the release of fuel. The remaining energy (40%) goes to the peripheral tissues and muscles, where insulin allows the energy to penetrate into the cells. If these cells are sensitive to leptin, they swallow all the 40% of calories without residue.
If they are resistant to leptin, the extra calories will go directly back to the liver to be placed in storage of fat in fat cells (or get stuck inside liver cells), because the insulin level is high. The more fat goes into storage, the higher the levels of leptin become over time. If the fat gets in the liver it causes a big immune response leading to many inflammatory chemicals.
Thus, obesity, particularly visceral, increases the flow to the liver of free fatty acids, while developing hepatic steatosis (first hit). In conditions of insulin resistance increased lipolysis in adipose tissue, and the excess FFA supplied to the liver. In the end, the amount of fatty acids in the hepatocytes increases dramatically, is formed by fatty degeneration of hepatocytes.
The literature describes four mechanisms of accumulation of fat in the liver: increase in intake of fat and free fatty acids (SFA) with food and capture them in the liver from the bloodstream; increased synthesis or inhibition of the processes of b-oxidation of FFA in mitochondria of hepatocytes, which contributes to the production of triglycerides (TG); impaired removal of TG from hepatocytes; carbohydrates coming to the liver from the bloodstream in excess amounts, can also be converted into fatty acids.
Increased influx of FFA and decrease their rate of oxidation leads to FFA esterification with excess formation of triglycerides in hepatocytes, and the secretion of increased amounts of lipoproteins of very low density (VLDL), contributing to the intensification of free radical oxidation of lipids and the accumulation of products of peroxidation (the"second push").
In high income FFA to the liver increases the role of microsomal fatty acid oxidation with participation of cytochrome P450 (CYP2E1 and CYP4A) and reduced Β-oxidation of FFA in mitochondria, which leads to the formation and accumulation of reactive oxygen species, possessing a direct cytotoxic effect on hepatocytes and initiates the process of lipid peroxidation.
Against the background of increasing secretion of proinflammatory cytokines by adipose tissue, primarily TNF-a, reactive oxygen species contribute to the uncoupling of oxidative phosphorylation, depletion of mitochondrial ATP and, ultimately, damage of hepatocytes and necrosis
Fifty two million nine hundred seventy eight thousand two hundred forty seven
The second shot (the fat becomes inflamed and oxidized) Simultaneously or sequentially developing oxidative stress — the "second strike" with the formation of the inflammatory response and development of steatohepatitis. This is due in large part to the fact that the functional ability of the mitochondria is depleted, it switches to the microsomal oxidation of lipids in the cytochrome, which leads to the formation of reactive oxygen species and increased production of proinflammatory cytokines with the formation of inflammation in the liver of hepatocyte death caused by cytotoxic effects of TNF-alpha1 — one of the main inducers of apoptosis. IL-6, -8 — a proinflammatory cytokines produced by adipose tissue, are "hepatoselective factors" and can induce the synthesis of proinflammatory proteins such as fibrinogen and C-reactive protein.
Thus, when the accumulation of fat in the liver reached a critical level, the fat becomes "bad" starts to do bad things, releasing inflammatory substances (IL-6 and TNF alpha). When you are resistant to leptin, the end result will be the packaging of calories in fat in one form or another LDL.
These portions LDL leaves the liver, because there is a physical limit to how much fat can be. If this process of creating LDL is chronic and suppresses the liver, fat accumulates inside the liver cells and causes the formation of significant amounts of reactive oxygen species (RoS). This inflammatory chemicals that insidiously kill cells and are the basis of all chronic diseases that you know.
The list of diseases and situations, which gives rise to "secondary" NAFLD and Nash, is very broad and includes: malabsorption syndrome, especially when operations for obesity intensive weight loss, long, unbalanced parenteral nutrition, disease accumulation.
Leptin and liver. Let's see, what is the role of leptin in the liver. The relationship of leptin with NAFLD was confirmed by subsequent research, which showed that both men and women have hyperleptinemia. But at the same time, leptin levels directly correlated only with the degree of hepatic steatosis, but was not an independent predictor of neither inflammatory process nor the severity of fibrosis.
Leptin increases the sensitivity of liver cells and muscle tissue to insulin. Excess of leptin leads to the suppression of insulin secretion, inhibits action of insulin on liver cells. It is established that in the liver leptin has the potential to inhibit gluconeogenesis by influencing the activity of fosfoenolpiruvatcarboksilaza enzyme limiting the rate of gluconeogenesis.
Fatty acid oxidation leptin enhances through the stimulation of AMP-activated protein kinase (AMPK). Hormone, limiting the accumulation of triglycerides in hepatocytes, prevents "lipotoxicity", and adjusts the degree of fibrosis in reparations. Leptin levels correlated with the severity of hepatic steatosis, but does not depend on the activity of inflammation or degree of fibrosis. The development of liver steatosis may be associated with leptinresistance.
According to numerous researches, devoted to studying cellular and molecular mechanisms underlying the profibrogenic effects of leptin, this adipokine exerts biological effects on various groups of cells, such as Kupffer cells, sinusoidal endothelial cells and myofibroblastic cells.
It enhances phagocytic activity and cytokine production copperhouse cells and macrophages, stimulates the proliferation of endothelial cells and their production of active forms of oxygen. In addition, leptin has a direct impact on stellate liver cells (HSC) which Express functionally active receptors satinovye.
Development of ObRb is significantly increased by transdifferentiation resting HSC in myofibroblastomas. Under the influence of leptin HSC produce increased amounts of procollagen type I and potentiate the effects of transforming growth factor beta-1 (TGF-b1). Moreover, under the action of leptin decreases the decay fibrosicistica extracellular collagen matrix (EKM), which is typical for the fibrogenic process .
Leptin plays an important role in the process of fibrogenesis in the liver. Some studies have shown profibrogenic action of this adipokine on the liver. Deficiency of leptin or latinovich receptors in laboratory animals was accompanied by significant reduction of fibrosis in experimental nonalcoholic steatohepatitis (Nash), intoxication with thioacetamide, prolonged exposure to carbon tetrachloride and other models of liver damage.
On the other hand, the introduction of leptin to animals with acute or chronic liver injury was accompanied by a significant increased production of procollagen type I and profibrogenic cytokine transforming growth factor 1 (TGF-1).
Was the role of leptin in process of angiogenesis in the liver. Activation latinovich receptors in stellate cells leads to enhanced development of vascular endothelial growth factor (VEGF), a potent stimulator of the formation of new blood vessels in tissue.
Neovascularization of liver tissue is another mechanism profibrogenic action of leptin and significantly affects the progression of liver damage in various chronic diseases. On the other hand, a proven link between angiogenesis and tumorigenesis suggests a possible involvement of leptin in the development of liver cancer.
Thirteen million one hundred fifty seven thousand three hundred eighty nine
Diagnosis of fatty liver disease
So, at the stage of nonalcoholic fatty liver disease the main symptom is hepatomegaly (discovered by accident or clinical examination). If increase in transaminase levels it is necessary to conduct virological research (which either confirm or reject viral hepatitis), as well as diagnosis of other forms of hepatitis: autoimmune, biliary, primary sclerosing cholangitis.
The diagnosis most often is made with ultrasound of the liver, in many cases, the patients previously did not even know about the existence of fatty degeneration of the liver. When ultrasound is observed a uniform enlargement of the liver, diffuse increase in its echogenicity (sometimes pronounced), with the preservation of its homogeneity (although the progression of the process there is a characteristic "grain" of the parenchyma, indicating the early development of steatohepatitis and hepatitis).
Ultrasound shows echogenicity, ultrasonic permeability, structure of the parenchyma etc., which may lead to the conclusion that the patient has a "diffuse changes of the liver".
The term "diffuse changes in the liver" implies a number of diseases. For this reason, a variety of diffuse liver disease from the point of view of the ultrasound diagnosis can be divided into mild and pronounced. The ultrasound picture may slightly vary depending on the stage and severity of the process, the type of fatty infiltration, as well as in combination of this disease with other accompanying changes of the liver.
When computed tomography revealed different degrees marked diffuse decrease in densitometric characteristics of the liver parenchyma (lower than 55 HU, sometimes up to negative values, corresponding to the density of the fat) generally increased size of the body.
Is it possible to detect constrained sites fatty infiltration, surrounded by normal liver tissue. Often local fat infiltration was observed in S4 of the liver, has a fairly smooth, straight outlines, the course of the vessels in the infiltrated fat tissue is not altered, mass-effect (body effect on surrounding structures).
Currently, the "gold standard" diagnosis of NAFLD is considered the liver biopsy in order to objectively diagnose NAFLD, to evaluate the extent to Nash, fibrosis stage, to predict the course of disease, monitor the effectiveness of treatment.
According to research, the practical significance of the diagnosis of NAFLD before biopsy using noninvasive methods is only 50%. Since 2005, in clinical practice for a comprehensive evaluation of the morphological changes in the liver with NAFLD scale is widely used NAS (NAFLD activity score) proposed by D. A. Kleiner
A marker of NAFLD can be content in the blood serum of fragments of the protein filaments of cytokeratin-18 (CK18-Asp396), resulting in its cleavage by activated kasasaki from hepatocytes during apoptosis. Increased levels of fragments of cytokeratin-18 is specific to steatohepatitis and to differentiate it from the steatosis. Specificity and sensitivity of this method make up 99.9% and 85,7% respectively.
Forty one million eight hundred eighty two thousand two hundred eighty three
Conclusion.1. You fat, if you have a fatty liver, regardless of your body weight.
2. Of the reasons leading to fatty liver damage from eating to toxic injury by alcohol. Not much difference in the course of the disease there.
3. Fatty liver causes the development of systemic inflammation which is the cause of many boleznei: from obesity to cardiovascular disease and cancer.
Gymnastics for eyes by Norbekov — reclaim your visual acuity!
WHAT you did not know the "healthy" vegetable oils
4. The condition of the liver can easily monitor and track your progress.
5. Fatty liver often completely asymptomatic and even doesn't show up on conventional tests. She, like hypertension, is a silent killer.published
Author: Andrey Blueskin
Source: www.beloveshkin.com/2015/07/leptinorezistentnost-i-zhirovaya-bolezn-pecheni.html
Almost every third person (according to others – every second!) found changes in the liver (fatty liver disease). Today we learn that resistance to the leptin begins with changes in the liver. And learn how dangerous fat in the liver, how it's measured and what it says.
To understand the relationship of stress, our reaction to it, it is important to know that stress is almost always associated with the accumulation of "bad" fat (the internal fat, visceral or abdominal fat). "Bad fat," causes inflammation, which increases stress and everything moves in a circle.
This mode of deficit, which manifests itself in all areas of human life: in mood, motivation, energy levels, appearance, activity, weight, disease, the psyche, and even in relationships with other people. As the proverb says, "with fat rage".But the "bad fat" is not always associated with excess weight. In addition, there are "good" fat, which is a great source of energy.
Forty five million two hundred four thousand three hundred eleven
Therefore, I will examine a number of cases in a not so obvious "bad" fat. Is fatty liver disease, skinny people with internal obesity and people of normal weight who are "fat inside". For balance, I will write about fat people who are healthy and not fat. Unfortunately, these nuances of the few who does, but they are critical to health. You consider yourself lean and not fat? Then we go to you! A more precisely, to your liver!
Fatty liver (fatty liver disease) is the Rubicon, which overeating and drinking turns into a real disease. The accumulation of fat in the liver called non-alcoholic fatty liver disease (NAFLD). I must say that there are alcoholic fatty liver disease, which is not much different (except for cause).
Have NAFLD, there are the following variants of the course:
steatosis (type 1) — the predominance of fatty degeneration of hepatocytes over all other morphological changes,
steatohepatitis (type 2) is expressed by inflammatory infiltrates in the stroma and the parenchyma with the presence of focal necrosis,
statefips (type 3) — predominance of fibrosis of the portal stroma, but without disruption of lobular structure, steatosis — a violation of the lobular structure of the liver with the presence of nodes regenerates. NAFLD can be a manifestation of various diseases and pathology
Nonalcoholic hepatic steatosis (nonalcoholic fatty liver disease (NAFLD), fatty liver, fatty liver, fatty infiltration) — primary liver disease or a syndrome generated by excess accumulation of fat (mainly triglycerides) in the liver. Normal liver contains about 5% fat. If we consider this nosology from a quantitative point of view, "fat" should be at least 5-10% of liver weight, or more than 5% of hepatocytes should contain lipids (histologically). It's a little! Ie, the disease is already active flows, if the fat has accumulated more than 5% of liver cells! Please note this fact!
Twenty four million seven hundred nine thousand four hundred seventy three
The course and manifestations of fatty liver disease.
1. Can occur bessimptomnom, found by accident.In many patients the liver detected by chance during examinations for other diseases.
2.Has mild symptoms.The disease is typically of long duration with minimal or moderate inflammation activity in the liver. In most patients, symptoms characteristic of liver disease are absent. Sometimes there are complaints of heaviness and discomfort in the right upper quadrant of the abdomen, aggravated by movement, fatigue, weakness, nausea. Often the disease is diagnosed accidentally during ultrasound examination of the liver after its enlargement and hyperechogenicity or "brightness" of the liver tissue due to diffuse fatty infiltration.
3. If you have normal tests, it does not exclude problems with the liver! Elevated levels of serum transaminases revealed only 20-21% of patients with NAFLD. However, normal levels of transaminases do not exclude veroyatnostnaya necrotic-inflammatory changes and fibrosis of the liver.
3. Happens in people with normal body weight. The increase in its incidence parallel to the obesity epidemic has allowed for the confirmation of fatty liver disease to use the body mass index (BMI). At the same time up to 25 % of patients with NAFLD may not be obese but have a clear laboratory evidence of IR.
4. Very slowly progressing. Usually steatosis is characterized by stable, non-progressive course. If to fatty infiltration joins the inflammatory process, that is developed steatohepatitis, the disease often progresses with the formation of liver fibrosis (30-40% of patients) and cirrhosis (approximately 10 %).
5. Fatty liver disease totally reversible! About this will be later. It should be noted the possibility of reverse development of nonalcoholic fatty disease on the background of reducing weight (and / or visceral fat).
6. Fatty liver disease is very common.The prevalence of non-alcoholic hepatic steatosis among residents of economically developed countries is an average of 2035%, non-alcoholic steatohepatitis and 3% [21, 29]. In the US hepatic steatosis have 34% of the adult population in Japan – 29% [10, 36]. In Russia, according to a screening program to identify the prevalence of NAFLD and its clinical forms, carried out in 2007 and engulfed 30754 people, NAFLD was diagnosed in 27% of patients.
7. Obesity is a problem with the liver is almost always.In obese patients the prevalence of different clinical forms of NAFLD are significantly higher than in the General population, and is, according to studies, up to 93%. According to Tarantino G. et al. (2007), steatosis is diagnosed in 10-25% of the U.S. population, including in 57-75% of patients with morbid (body mass index >30-35) obese and nearly 100% of with obesity and type 2 diabetes. It is noted feedback: patients with NAFLD revealed obesity in 30-100% of cases, type 2 diabetes in 10 to 75%, hyperlipidemia in 20-92% of cases.
Sixty three million nine hundred one thousand four
How is fatty liver disease? For the development of fatty disease need two strokes. The first shot is poor nutrition. When the fat accumulates in the liver. The second blow is inflammation and oxidation (oxidative stress). Fat is oxidized and becomes "bad" fat, i.e., produces compounds that trigger inflammation.
Blow to the liver can be applied not only fast food but also alcohol. Alcoholic fatty liver disease like non-alcoholic, and the result is the same! Traced a direct correlation of the type of liver disease the dose of alcohol consumed daily.
It should be noted that the type of drink is not important, important is the amount of alcohol. It was noted that alcohol is the main cause of liver disease in Europe. Perhaps a combination of alcoholic liver disease and NAFLD. Fatty degeneration of the liver occurs more frequently in individuals with obesity, history of alcohol abuse. Safe dose of alcohol that do not cause the progression of NAFLD has not been established.
Forty three million twenty five thousand five hundred ninety eight
The first blow (fat accumulates) When people eat a meal, about 60% of the calories is deposited in the liver to provide the tissues with energy in between meals. Another hormone, glucagon, mediates the release of fuel. The remaining energy (40%) goes to the peripheral tissues and muscles, where insulin allows the energy to penetrate into the cells. If these cells are sensitive to leptin, they swallow all the 40% of calories without residue.
If they are resistant to leptin, the extra calories will go directly back to the liver to be placed in storage of fat in fat cells (or get stuck inside liver cells), because the insulin level is high. The more fat goes into storage, the higher the levels of leptin become over time. If the fat gets in the liver it causes a big immune response leading to many inflammatory chemicals.
Thus, obesity, particularly visceral, increases the flow to the liver of free fatty acids, while developing hepatic steatosis (first hit). In conditions of insulin resistance increased lipolysis in adipose tissue, and the excess FFA supplied to the liver. In the end, the amount of fatty acids in the hepatocytes increases dramatically, is formed by fatty degeneration of hepatocytes.
The literature describes four mechanisms of accumulation of fat in the liver: increase in intake of fat and free fatty acids (SFA) with food and capture them in the liver from the bloodstream; increased synthesis or inhibition of the processes of b-oxidation of FFA in mitochondria of hepatocytes, which contributes to the production of triglycerides (TG); impaired removal of TG from hepatocytes; carbohydrates coming to the liver from the bloodstream in excess amounts, can also be converted into fatty acids.
Increased influx of FFA and decrease their rate of oxidation leads to FFA esterification with excess formation of triglycerides in hepatocytes, and the secretion of increased amounts of lipoproteins of very low density (VLDL), contributing to the intensification of free radical oxidation of lipids and the accumulation of products of peroxidation (the"second push").
In high income FFA to the liver increases the role of microsomal fatty acid oxidation with participation of cytochrome P450 (CYP2E1 and CYP4A) and reduced Β-oxidation of FFA in mitochondria, which leads to the formation and accumulation of reactive oxygen species, possessing a direct cytotoxic effect on hepatocytes and initiates the process of lipid peroxidation.
Against the background of increasing secretion of proinflammatory cytokines by adipose tissue, primarily TNF-a, reactive oxygen species contribute to the uncoupling of oxidative phosphorylation, depletion of mitochondrial ATP and, ultimately, damage of hepatocytes and necrosis
Fifty two million nine hundred seventy eight thousand two hundred forty seven
The second shot (the fat becomes inflamed and oxidized) Simultaneously or sequentially developing oxidative stress — the "second strike" with the formation of the inflammatory response and development of steatohepatitis. This is due in large part to the fact that the functional ability of the mitochondria is depleted, it switches to the microsomal oxidation of lipids in the cytochrome, which leads to the formation of reactive oxygen species and increased production of proinflammatory cytokines with the formation of inflammation in the liver of hepatocyte death caused by cytotoxic effects of TNF-alpha1 — one of the main inducers of apoptosis. IL-6, -8 — a proinflammatory cytokines produced by adipose tissue, are "hepatoselective factors" and can induce the synthesis of proinflammatory proteins such as fibrinogen and C-reactive protein.
Thus, when the accumulation of fat in the liver reached a critical level, the fat becomes "bad" starts to do bad things, releasing inflammatory substances (IL-6 and TNF alpha). When you are resistant to leptin, the end result will be the packaging of calories in fat in one form or another LDL.
These portions LDL leaves the liver, because there is a physical limit to how much fat can be. If this process of creating LDL is chronic and suppresses the liver, fat accumulates inside the liver cells and causes the formation of significant amounts of reactive oxygen species (RoS). This inflammatory chemicals that insidiously kill cells and are the basis of all chronic diseases that you know.
The list of diseases and situations, which gives rise to "secondary" NAFLD and Nash, is very broad and includes: malabsorption syndrome, especially when operations for obesity intensive weight loss, long, unbalanced parenteral nutrition, disease accumulation.
Leptin and liver. Let's see, what is the role of leptin in the liver. The relationship of leptin with NAFLD was confirmed by subsequent research, which showed that both men and women have hyperleptinemia. But at the same time, leptin levels directly correlated only with the degree of hepatic steatosis, but was not an independent predictor of neither inflammatory process nor the severity of fibrosis.
Leptin increases the sensitivity of liver cells and muscle tissue to insulin. Excess of leptin leads to the suppression of insulin secretion, inhibits action of insulin on liver cells. It is established that in the liver leptin has the potential to inhibit gluconeogenesis by influencing the activity of fosfoenolpiruvatcarboksilaza enzyme limiting the rate of gluconeogenesis.
Fatty acid oxidation leptin enhances through the stimulation of AMP-activated protein kinase (AMPK). Hormone, limiting the accumulation of triglycerides in hepatocytes, prevents "lipotoxicity", and adjusts the degree of fibrosis in reparations. Leptin levels correlated with the severity of hepatic steatosis, but does not depend on the activity of inflammation or degree of fibrosis. The development of liver steatosis may be associated with leptinresistance.
According to numerous researches, devoted to studying cellular and molecular mechanisms underlying the profibrogenic effects of leptin, this adipokine exerts biological effects on various groups of cells, such as Kupffer cells, sinusoidal endothelial cells and myofibroblastic cells.
It enhances phagocytic activity and cytokine production copperhouse cells and macrophages, stimulates the proliferation of endothelial cells and their production of active forms of oxygen. In addition, leptin has a direct impact on stellate liver cells (HSC) which Express functionally active receptors satinovye.
Development of ObRb is significantly increased by transdifferentiation resting HSC in myofibroblastomas. Under the influence of leptin HSC produce increased amounts of procollagen type I and potentiate the effects of transforming growth factor beta-1 (TGF-b1). Moreover, under the action of leptin decreases the decay fibrosicistica extracellular collagen matrix (EKM), which is typical for the fibrogenic process .
Leptin plays an important role in the process of fibrogenesis in the liver. Some studies have shown profibrogenic action of this adipokine on the liver. Deficiency of leptin or latinovich receptors in laboratory animals was accompanied by significant reduction of fibrosis in experimental nonalcoholic steatohepatitis (Nash), intoxication with thioacetamide, prolonged exposure to carbon tetrachloride and other models of liver damage.
On the other hand, the introduction of leptin to animals with acute or chronic liver injury was accompanied by a significant increased production of procollagen type I and profibrogenic cytokine transforming growth factor 1 (TGF-1).
Was the role of leptin in process of angiogenesis in the liver. Activation latinovich receptors in stellate cells leads to enhanced development of vascular endothelial growth factor (VEGF), a potent stimulator of the formation of new blood vessels in tissue.
Neovascularization of liver tissue is another mechanism profibrogenic action of leptin and significantly affects the progression of liver damage in various chronic diseases. On the other hand, a proven link between angiogenesis and tumorigenesis suggests a possible involvement of leptin in the development of liver cancer.
Thirteen million one hundred fifty seven thousand three hundred eighty nine
Diagnosis of fatty liver disease
So, at the stage of nonalcoholic fatty liver disease the main symptom is hepatomegaly (discovered by accident or clinical examination). If increase in transaminase levels it is necessary to conduct virological research (which either confirm or reject viral hepatitis), as well as diagnosis of other forms of hepatitis: autoimmune, biliary, primary sclerosing cholangitis.
The diagnosis most often is made with ultrasound of the liver, in many cases, the patients previously did not even know about the existence of fatty degeneration of the liver. When ultrasound is observed a uniform enlargement of the liver, diffuse increase in its echogenicity (sometimes pronounced), with the preservation of its homogeneity (although the progression of the process there is a characteristic "grain" of the parenchyma, indicating the early development of steatohepatitis and hepatitis).
Ultrasound shows echogenicity, ultrasonic permeability, structure of the parenchyma etc., which may lead to the conclusion that the patient has a "diffuse changes of the liver".
The term "diffuse changes in the liver" implies a number of diseases. For this reason, a variety of diffuse liver disease from the point of view of the ultrasound diagnosis can be divided into mild and pronounced. The ultrasound picture may slightly vary depending on the stage and severity of the process, the type of fatty infiltration, as well as in combination of this disease with other accompanying changes of the liver.
When computed tomography revealed different degrees marked diffuse decrease in densitometric characteristics of the liver parenchyma (lower than 55 HU, sometimes up to negative values, corresponding to the density of the fat) generally increased size of the body.
Is it possible to detect constrained sites fatty infiltration, surrounded by normal liver tissue. Often local fat infiltration was observed in S4 of the liver, has a fairly smooth, straight outlines, the course of the vessels in the infiltrated fat tissue is not altered, mass-effect (body effect on surrounding structures).
Currently, the "gold standard" diagnosis of NAFLD is considered the liver biopsy in order to objectively diagnose NAFLD, to evaluate the extent to Nash, fibrosis stage, to predict the course of disease, monitor the effectiveness of treatment.
According to research, the practical significance of the diagnosis of NAFLD before biopsy using noninvasive methods is only 50%. Since 2005, in clinical practice for a comprehensive evaluation of the morphological changes in the liver with NAFLD scale is widely used NAS (NAFLD activity score) proposed by D. A. Kleiner
A marker of NAFLD can be content in the blood serum of fragments of the protein filaments of cytokeratin-18 (CK18-Asp396), resulting in its cleavage by activated kasasaki from hepatocytes during apoptosis. Increased levels of fragments of cytokeratin-18 is specific to steatohepatitis and to differentiate it from the steatosis. Specificity and sensitivity of this method make up 99.9% and 85,7% respectively.
Forty one million eight hundred eighty two thousand two hundred eighty three
Conclusion.1. You fat, if you have a fatty liver, regardless of your body weight.
2. Of the reasons leading to fatty liver damage from eating to toxic injury by alcohol. Not much difference in the course of the disease there.
3. Fatty liver causes the development of systemic inflammation which is the cause of many boleznei: from obesity to cardiovascular disease and cancer.
Gymnastics for eyes by Norbekov — reclaim your visual acuity!
WHAT you did not know the "healthy" vegetable oils
4. The condition of the liver can easily monitor and track your progress.
5. Fatty liver often completely asymptomatic and even doesn't show up on conventional tests. She, like hypertension, is a silent killer.published
Author: Andrey Blueskin
Source: www.beloveshkin.com/2015/07/leptinorezistentnost-i-zhirovaya-bolezn-pecheni.html