441
What is a splenectomy
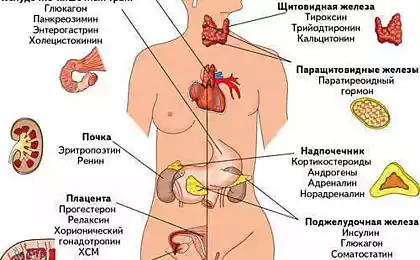
Splenectomy is a surgical procedure that involves total or partial removal of the spleen. The spleen plays an important role in the functioning of the immune system, helping it to fight off bacteria and infections. It also contributes to the filtering blood and regulates the blood flow to the liver. If the spleen is damaged or diseased, it may be necessary to splenectomy.
Forty two million four hundred seventy seven thousand six hundred ninety five
Splenectomy is performed under General anesthesia, i.e. the patient in this operation is asleep. Laparoscopic splenectomy involves the use of a thin instrument with a camera and a light on the end called a laparoscope. The surgeon leads a laparoscope through a small incision in the abdomen, while through the other small incisions surgical instruments are inserted. Patients undergoing splenectomy laparoscopical usually recover faster than those who undergo open splenectomy.
Open splenectomy suggests the need for a large incision in the center of the abdomen or on the left side of the abdomen under the ribs.
The surgeon removes the spleen through the incision and then applies stitches to close the wound. Patients who required splenectomy because of spleen cancer, often undergo open surgery so that the surgeon can examine the lymph nodes in the stomach for signs of cancer. Infected lymph nodes may be removed also during this procedure. If damaged or diseased spleen is not all, you can only delete part of it. This reduces the risk of infection, as the spleen helps the immune system fight bacteria in the body. Partial splenectomy often provides pain relief to patients with an enlarged spleen.
The most common risks associated with splenectomy is the development of internal bacterial infection which can spread throughout the body.
After removal of the spleen, the body's ability to filter blood of bacteria and viruses is reduced. In children the risk of infection is higher than in adults, with the greatest likelihood of infection observed during the first two years after surgery. This risk can be minimized through the implementation before the procedure of vaccination against certain infections.
Other complications of splenectomy include reactions to anesthesia, breathing problems, blood clots, substantial blood loss and infection. Patients can minimize the risk of infections, eating before and after surgery, a healthy diet, refraining from tobacco and alcohol, and properly caring for the wound. Splenectomy can cause damage to adjacent organs such as the stomach, pancreas and colon. The risk of damage to other organs is minimal if the operation is conducted by an experienced surgeon.
A full recovery after splenectomy is usually required from four to six weeks.
At the hospital, most patients spend less than a week. To complete wound healing, patients should refrain from lifting heavy objects or making other movements, leading to tension on the wound. Normally, surgeons provide patients with detailed instructions on caring for the surgical wound, including tips for washing and changing bandages.
Source: globalscience.ru
Forty two million four hundred seventy seven thousand six hundred ninety five
Splenectomy is performed under General anesthesia, i.e. the patient in this operation is asleep. Laparoscopic splenectomy involves the use of a thin instrument with a camera and a light on the end called a laparoscope. The surgeon leads a laparoscope through a small incision in the abdomen, while through the other small incisions surgical instruments are inserted. Patients undergoing splenectomy laparoscopical usually recover faster than those who undergo open splenectomy.
Open splenectomy suggests the need for a large incision in the center of the abdomen or on the left side of the abdomen under the ribs.
The surgeon removes the spleen through the incision and then applies stitches to close the wound. Patients who required splenectomy because of spleen cancer, often undergo open surgery so that the surgeon can examine the lymph nodes in the stomach for signs of cancer. Infected lymph nodes may be removed also during this procedure. If damaged or diseased spleen is not all, you can only delete part of it. This reduces the risk of infection, as the spleen helps the immune system fight bacteria in the body. Partial splenectomy often provides pain relief to patients with an enlarged spleen.
The most common risks associated with splenectomy is the development of internal bacterial infection which can spread throughout the body.
After removal of the spleen, the body's ability to filter blood of bacteria and viruses is reduced. In children the risk of infection is higher than in adults, with the greatest likelihood of infection observed during the first two years after surgery. This risk can be minimized through the implementation before the procedure of vaccination against certain infections.
Other complications of splenectomy include reactions to anesthesia, breathing problems, blood clots, substantial blood loss and infection. Patients can minimize the risk of infections, eating before and after surgery, a healthy diet, refraining from tobacco and alcohol, and properly caring for the wound. Splenectomy can cause damage to adjacent organs such as the stomach, pancreas and colon. The risk of damage to other organs is minimal if the operation is conducted by an experienced surgeon.
A full recovery after splenectomy is usually required from four to six weeks.
At the hospital, most patients spend less than a week. To complete wound healing, patients should refrain from lifting heavy objects or making other movements, leading to tension on the wound. Normally, surgeons provide patients with detailed instructions on caring for the surgical wound, including tips for washing and changing bandages.
Source: globalscience.ru