414
Causes of male infertility: deficiency regimen, leptin, insulin
Recently, we have seen an increase in the frequency of infertility. I talked earlier about how leptin problems and insulin resistance are related to female infertility, now let’s talk about male. Let me remind you that the reproductive sphere is one of the most energy-intensive, so one of the first to suffer from a deficit regime.
Decreased libido and fertility in a deficit regime is a natural protective biological response. Back to male infertility and metabolic syndrome (deficiency regimen). The clinical significance of obesity in men is much higher than in women: it is much more difficult to treat with traditional methods, leads to an acceleration of the development and progression of cardiovascular diseases, leading to a decrease in the average life expectancy in men compared to women by 8-12 years. The mechanisms of the negative impact of overweight and obesity on male reproduction are quite diverse.
Infertility is the inability of a somatically healthy couple of reproductive age who do not use contraception to achieve conception within 12 months of regular sexual activity. The frequency of infertile marriages in the world is growing catastrophically: in Europe and the United States it is 15%, in Canada – 17%, and in Russia it is approaching 20%. Recently, male infertility is equal in frequency with female - the frequency of the "male" factor in family infertility reaches 40-50%.
Causes of male infertility: leptin
With obesity, there is an increase in the level of leptin in the blood (a marker of the volume of adipocytes and activity of adipocytes), which was called "leptin resistance", while leptin induces clinical androgen deficiency by reducing the sensitivity of androgen receptors to testosterone and blocking the synthesis of luteinizing hormone in the pituitary gland, on the one hand, and increasing the aromatization of testosterone on the periphery in estradiol under the influence of aromatase of adiol tissue - on the other.
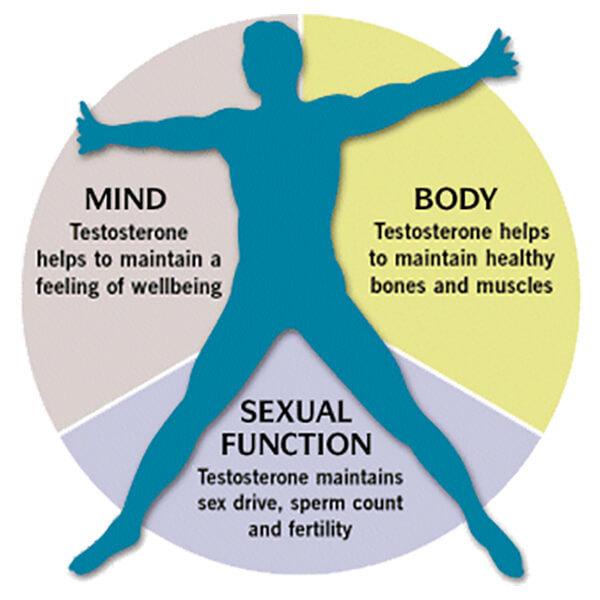
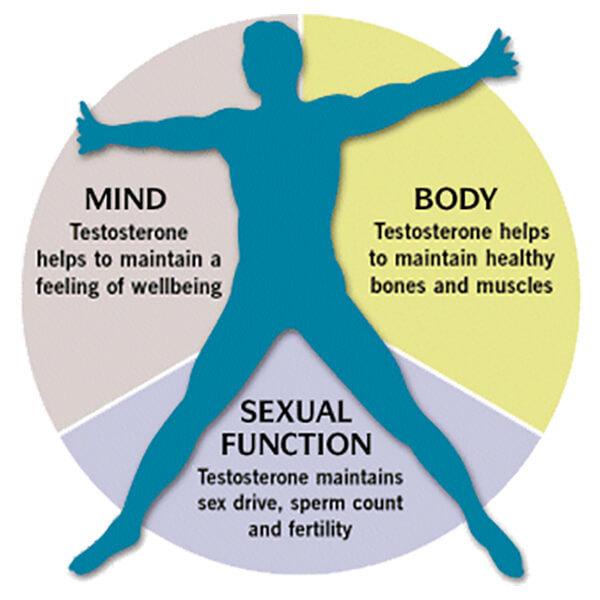
The synergy of the effects of both pathological processes leads to profound disorders of the reproductive system of obese men, associated not only with oxidative stress against the background of an excess of free fatty acids and triglycerides in the blood, but also due to a deficiency of testosterone - a key sex steroid necessary for normal spermatogenesis.
D. Goulis and B. Tarlatzis (2008) believe that obesity leads to a decrease in the level of total testosterone and globulin, which binds sex steroids, which becomes a manifestation of the negative effect of adipose tissue on testicular function. Although the exact pathophysiological mechanisms of this interaction remain unclear, it is suggested that leptin, resistin, and ghrelin (adipose tissue hormones) play an important role in the interaction between obesity and testicular dysfunction.
On the other hand, androgenic deficiency arising from obesity exacerbates insulin resistance, which is the main pathophysiological mechanism, along with obesity, that triggers systemic oxidative stress leading to pathozoospermia. P.Mah and G.Wittert (2010) cite similar findings that obesity in men is significantly associated with low total and free blood testosterone levels, which in turn increase the risk of developing IR and type 2 diabetes.
Hypogonadism in obese men can also be a consequence of systemic chronic inflammation, which naturally develops against the background of obesity, and often associated with obesity hormone D deficiency, which is extremely necessary for the synthesis of testosterone and maintenance of reproductive function in men. With obesity in Leydig cells, a violation of the cholesterol transformation chain under the influence of cytochrome P450 is observed due to the ability of TNF-a and IL-1 to inhibit steroidogenesis, which leads to a decrease in testosterone synthesis.
Disorders of testosterone synthesis in obesity in men constitute today the “endocrinological axiom” of andrology, since, on the one hand, despite the fact that testosterone is not a direct inducer of spermatogenesis, it is absolutely necessary for its maintenance, on the other hand, the pathogenetic relationship of androgenic deficiency and obesity in men is reliably proven today.
This is extremely important for understanding the pathophysiological systemic effects of obesity, which are currently described by the term “lipotoxicity of adipose tissue” and which are most actively involved in the induction and progression of systemic oxidative stress with negative effects on spermatogenic and steroidogenic function.
An excess of free fatty acids and triglycerides in the blood during obesity causes the start of systemic oxidative stress, which leads to an excessive accumulation of free radicals in the cells and tissues of various organs, including skeletal muscles, heart myocytes, hepatocytes, pancreatic b-cells, renal and testicular epithelium, which leads to chronic cell dysfunction due to their damage. Triglycerides have toxicity due to unesterified long-chain fatty acids and their products (ceramides and diacylglycerols).
Mitochondrial dysfunction of the testicular epithelium, induced by unesterified long-chain fatty acids, is the main mechanism of impaired testicular structure and function in men with obesity, and the simultaneous decrease in the content of antioxidants in the systemic bloodstream aggravates and contributes to the further progression of oxidative stress.
The growth of infertility in industrialized countries is associated with the impact on the reproductive system of a number of adverse medical, nutritional and psychological factors leading to an increase in the overall morbidity of the modern population, among which currently the undisputed leader is obesity, often leading to type 2 diabetes (Type 2 diabetes) and and androgen deficiency in men and, as a result, significantly increasing the risk of oxidative (and inflammatory) sperm stress.
In routine andrological practice, there are no standard recommendations for screening-diagnosis of oxidative sperm stress in infertile men, but it is clear that the earlier the oxidative stress of sperm is identified and corrected, the less reproductive losses a man suffers.
Causes of male infertility: inflammatory-oxidative stress
It is extremely important to bear in mind that oxidative stress of sperm is reliably present not only in men with urological pathology (for example, with varicocele or inflammatory diseases of the prostate gland), but also almost always occurs with obesity, diabetes mellitus or androgenic deficiency, regardless of the presence or absence of pathology of the reproductive system in an infertile man.
Obesity is a proven systemic factor that negatively affects male reproduction through the early initiation of systemic oxidative stress, leading to excessive accumulation of oxygen free radicals in the ejaculate to sperm DNA fragmentation (sperm oxidative stress). Less known to urologists-andrologists metabolic phenomenon of insulin resistance (IR), which naturally sooner or later develops with the progression of obesity and which is characterized by a violation of tissue sensitivity to glucose, which leads to mitochondrial sperm insufficiency (all the same sperm oxidative stress).
And if today many doctors associate reproductive losses with obesity and recommend to their infertile patients with overweight to reduce it, then early diagnosis and correction of IR has not yet become the norm of examination of every infertile man with obesity, although it is IR that is the earliest (preclinical) and therefore reversible stage of type 2 diabetes mellitus, which can and should be actively detected in all men with infertility against the background of obesity. IR leads to glycolytic stress of the nerve endings, i.e., in fact, initiates metabolic urogenital neuropathy, leading to a violation of ejacular dynamics and fertile properties of the ejaculate.
Causes and mechanism of infertility development
Reducing testosterone levels (androgen deficiency) is increasingly seen today as a possible new and pathogenetically important component of MS in men, since it has been proven that the frequency and severity of androgen deficiency in men is in reliable feedback not only with the frequency and severity of obesity, but also insulin resistance and type 2 diabetes.
Not only obesity (BMI > 30), but even just excess weight (BMI = 25-29) in men significantly increase the frequency of infertility compared to men with a normal body mass index (BMI = 20-22.4). Obesity worsens the quality of the ejaculate by reducing its volume and increasing the frequency of sperm DNA damage. Type 2 diabetes mellitus - a frequent companion of obesity - can lead to the development of ejaculatory dysfunction, which can also cause a violation of the delivery of sperm into the female genital tract.

Recently, the oxidative theory of the pathogenesis of male infertility has become very popular, with metabolic syndrome playing a major role in it. The components of MS lead to an increase in free radicals of active oxygen in the ejaculate, followed by hyperperoxidation of sperm membranes and damage to their DNA.
Thus, the presence of MS in a man of any age with infertility is an indication not only to clarify the causes of hormonal metabolic disorders, but also to actively search for oxidative sperm stress.
Modern literary sources associate a decrease in reproductive potential in obese men with such pathophysiological phenomena as a deficiency of sex hormones (primarily testosterone), hormone D, endothelial dysfunction and a deficiency of regional circulation, including testicular blood flow, against the background of pronounced vasoconstriction due to a deficiency of nitric oxide (NO); excessive activity of the prooxidant blood system; excess of triglycerides and free fatty acids, which ultimately lead to a decrease in the number of sexually morphic cells, and permiosmosis.
According to the generally accepted point of view, oxidative stress of sperm develops when the dynamic balance between oxidants and antioxidants in the seminal plasma is disturbed, and its frequency in male infertility, according to various authors, reaches 30-80%. Hyperproduction of reactive oxygen species - free radicals - can be detected in many pathological conditions, both related to the reproductive system (local factors - inflammation of the genital appendage glands, varicocele, urogenital infections), and not directly related to it, which play the role of systemic mechanisms of oxidative stress of sperm (any psycho-emotional stress, diabetes type 2): obesity, systemic chronic inflammation, smoking, poor ecology, lifestyle and nutrition.
Thus, at present, the explanation of the influence of many negative pathophysiological mechanisms of obesity (systemic chronic inflammation, dyslipidemia, disorders of carbohydrate metabolism, androgen deficiency, fat lipotoxicity, etc.) on spermatogenesis is directly or indirectly associated with the theory of oxidative stress of spermatozoa, which they induce during the entire time while a man has obesity, the persistence and development of which they contribute to the progression of obesity in an infertile man.
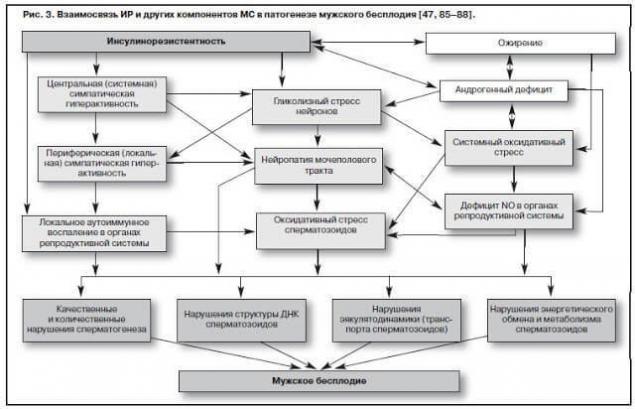
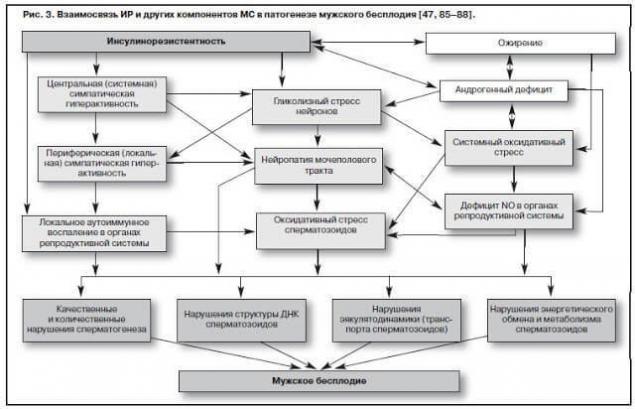
Causes of male infertility: insulin resistance
Insulin resistance, or hyperinsulinemia, being a key pathogenetic factor of MS, is a complex of compensatory and adaptive reactions that develop against the background of obesity, often associated with androgen deficiency in men.
With the development and progression of obesity, the expression of the insulin receptor gene decreases sharply, which leads to a decrease in the density of receptors on the cell surface and the emergence of insulin resistance, and a simultaneous increase in the level of the main hormone of adipose tissue - leptin - destroys the functional connection between the pituitary gland and gonads, which is the pathogenetic basis for the formation and progression of androgenic deficiency in men simultaneously with the progression of obesity and IR.
Developing IR is accompanied by hyperinsulinemia, which in this case ensures the maintenance of the efficiency of carbohydrate metabolism, viability and cell division. IR is the earliest and therefore potentially reversible stage of type 2 diabetes, so its early detection in any somatic diseases in obese men is an important preventive measure against type 2 diabetes and and androgen deficiency.
Early diagnosis of IR is indicated for all men of reproductive age with obesity and any other components of MS, since male infertility (especially the so-called idiopathic) can be pathogenetically associated with IR, the mechanisms of which in this case can be reduced to the following:
Early disruption of the structure and function of nervous tissue (glycolysis stress), while initial damage is noted in the smallest peripheral nerve endings of the organs of the urogenital system (kidneys, penis, prostate gland, testicles) (the effect of induction and progression of urogenital metabolic neuropathy).
Neuropathy leads to systemic and local vasoconstrictor-type reactions and ends with the development of endothelial dysfunction due to a deficiency of the main vasodilator - nitric oxide (since 90% of nitric oxide synthesis occurs not in the endothelium, but in the terminals of the nerve endings of blood vessels).
Any neuropathy is associated with the activation of the lipid peroxidation system - systemic oxidative stress, which is a powerful damaging factor for testicular parenchyma, which ends with impaired spermatogenesis (infertility) and (or) steroidogenesis (androgenic deficiency). A variant of this systemic effect of IR is oxidative (oxidative) sperm stress.
IR and obesity, being key components of MS, initiate systemic chronic inflammation (cytokine cascade reactions), which are actively involved in the implementation of another mechanism of damaging action on testicular tissue (an analogue of oxidative stress) - renal lipotoxicity, leading to a violation of the DNA structure of sperm.
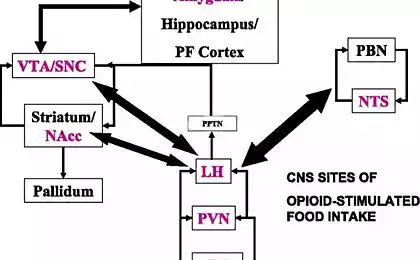
In addition, hyperinsulinemia leads to an increase in systemic sympathetic activity through impaired glucose metabolism in ventromedial hypothalamic neurons, which is accompanied by increased activity of a-adrenoreceptors of the urogenital tract (autonomous sympathetic hyperactivity, or neuropathy) and triggers systemic oxidative stress. M.Sankhla et al. (2012) in a survey of 120 men aged 17-26 years with obesity and infertility revealed a significant increase in the level of malondialdehyde (a marker of systemic oxidative stress) with an increase in BMI (p<0 div="nbsp=">>
Among the mechanisms of impaired fertility in patients with disorders of carbohydrate metabolism, some authors call the characteristic for this group of patients lesion of the appendages of the testicles, which can lead to impaired sperm transport, as well as urogenital neuropathy (glycolysis stress of neurons), oxidative stress, leading to damage to the nuclear and mitochondrial DNA of sperm and their increased immobilization, as well as NO deficiency due to androgenic insufficiency and neuropathy, since 90% of NO synthesized in the vascular wall is of neuronal origin.
Conclusion
Thus, infertile young men with obesity, in the absence of caution from the attending physician, there is always a danger of hypodiagnosis of the key component of MS - IR, which has a significant negative effect on spermatogenesis. From this point of view, it seems to us that the frequency of idiopathic infertility due to early detection of IR could be lower than it is commonly said. Idiopathic infertility today is most often infertility without a clear urological cause, since the problems of reproduction in our country are traditionally attributed to the competence of urologists. .
These are the imperatives of the twenty-first century – the age of pathogenetic and preventive medicine and interdisciplinary interactions. Therefore, a modern urologist from a surgeon should turn into a clinician and actively interact with related specialists (endocrinologists, therapists, neurologists).
Meridional tapping: The technique of emotional freedom
Key to the muscles of the cortex: lumbar muscle (psoas)
If this does not happen, then there is a high probability that in solving male reproductive problems in our country, the urologist will soon be a simple dispatcher who prescribes a couple exclusively referrals to reproductive clinics, since we are not able to stop the global epidemic of “diseases of civilization”, which today are the leading systemic pathophysiological initiators of oxidative sperm stress, clinically ending in male infertility. published
Author: Andrey Beloveskin
P.S. And remember, just by changing your consciousness – together we change the world!
Source: www.beloveshkin.com/2015/08/prichiny-muzhskogo-besplodiya-rezhim-deficita-leptin-insulin.html
Decreased libido and fertility in a deficit regime is a natural protective biological response. Back to male infertility and metabolic syndrome (deficiency regimen). The clinical significance of obesity in men is much higher than in women: it is much more difficult to treat with traditional methods, leads to an acceleration of the development and progression of cardiovascular diseases, leading to a decrease in the average life expectancy in men compared to women by 8-12 years. The mechanisms of the negative impact of overweight and obesity on male reproduction are quite diverse.
Infertility is the inability of a somatically healthy couple of reproductive age who do not use contraception to achieve conception within 12 months of regular sexual activity. The frequency of infertile marriages in the world is growing catastrophically: in Europe and the United States it is 15%, in Canada – 17%, and in Russia it is approaching 20%. Recently, male infertility is equal in frequency with female - the frequency of the "male" factor in family infertility reaches 40-50%.
Causes of male infertility: leptin
With obesity, there is an increase in the level of leptin in the blood (a marker of the volume of adipocytes and activity of adipocytes), which was called "leptin resistance", while leptin induces clinical androgen deficiency by reducing the sensitivity of androgen receptors to testosterone and blocking the synthesis of luteinizing hormone in the pituitary gland, on the one hand, and increasing the aromatization of testosterone on the periphery in estradiol under the influence of aromatase of adiol tissue - on the other.
The synergy of the effects of both pathological processes leads to profound disorders of the reproductive system of obese men, associated not only with oxidative stress against the background of an excess of free fatty acids and triglycerides in the blood, but also due to a deficiency of testosterone - a key sex steroid necessary for normal spermatogenesis.
D. Goulis and B. Tarlatzis (2008) believe that obesity leads to a decrease in the level of total testosterone and globulin, which binds sex steroids, which becomes a manifestation of the negative effect of adipose tissue on testicular function. Although the exact pathophysiological mechanisms of this interaction remain unclear, it is suggested that leptin, resistin, and ghrelin (adipose tissue hormones) play an important role in the interaction between obesity and testicular dysfunction.
On the other hand, androgenic deficiency arising from obesity exacerbates insulin resistance, which is the main pathophysiological mechanism, along with obesity, that triggers systemic oxidative stress leading to pathozoospermia. P.Mah and G.Wittert (2010) cite similar findings that obesity in men is significantly associated with low total and free blood testosterone levels, which in turn increase the risk of developing IR and type 2 diabetes.
Hypogonadism in obese men can also be a consequence of systemic chronic inflammation, which naturally develops against the background of obesity, and often associated with obesity hormone D deficiency, which is extremely necessary for the synthesis of testosterone and maintenance of reproductive function in men. With obesity in Leydig cells, a violation of the cholesterol transformation chain under the influence of cytochrome P450 is observed due to the ability of TNF-a and IL-1 to inhibit steroidogenesis, which leads to a decrease in testosterone synthesis.
Disorders of testosterone synthesis in obesity in men constitute today the “endocrinological axiom” of andrology, since, on the one hand, despite the fact that testosterone is not a direct inducer of spermatogenesis, it is absolutely necessary for its maintenance, on the other hand, the pathogenetic relationship of androgenic deficiency and obesity in men is reliably proven today.
This is extremely important for understanding the pathophysiological systemic effects of obesity, which are currently described by the term “lipotoxicity of adipose tissue” and which are most actively involved in the induction and progression of systemic oxidative stress with negative effects on spermatogenic and steroidogenic function.
An excess of free fatty acids and triglycerides in the blood during obesity causes the start of systemic oxidative stress, which leads to an excessive accumulation of free radicals in the cells and tissues of various organs, including skeletal muscles, heart myocytes, hepatocytes, pancreatic b-cells, renal and testicular epithelium, which leads to chronic cell dysfunction due to their damage. Triglycerides have toxicity due to unesterified long-chain fatty acids and their products (ceramides and diacylglycerols).
Mitochondrial dysfunction of the testicular epithelium, induced by unesterified long-chain fatty acids, is the main mechanism of impaired testicular structure and function in men with obesity, and the simultaneous decrease in the content of antioxidants in the systemic bloodstream aggravates and contributes to the further progression of oxidative stress.
The growth of infertility in industrialized countries is associated with the impact on the reproductive system of a number of adverse medical, nutritional and psychological factors leading to an increase in the overall morbidity of the modern population, among which currently the undisputed leader is obesity, often leading to type 2 diabetes (Type 2 diabetes) and and androgen deficiency in men and, as a result, significantly increasing the risk of oxidative (and inflammatory) sperm stress.
In routine andrological practice, there are no standard recommendations for screening-diagnosis of oxidative sperm stress in infertile men, but it is clear that the earlier the oxidative stress of sperm is identified and corrected, the less reproductive losses a man suffers.
Causes of male infertility: inflammatory-oxidative stress
It is extremely important to bear in mind that oxidative stress of sperm is reliably present not only in men with urological pathology (for example, with varicocele or inflammatory diseases of the prostate gland), but also almost always occurs with obesity, diabetes mellitus or androgenic deficiency, regardless of the presence or absence of pathology of the reproductive system in an infertile man.
Obesity is a proven systemic factor that negatively affects male reproduction through the early initiation of systemic oxidative stress, leading to excessive accumulation of oxygen free radicals in the ejaculate to sperm DNA fragmentation (sperm oxidative stress). Less known to urologists-andrologists metabolic phenomenon of insulin resistance (IR), which naturally sooner or later develops with the progression of obesity and which is characterized by a violation of tissue sensitivity to glucose, which leads to mitochondrial sperm insufficiency (all the same sperm oxidative stress).
And if today many doctors associate reproductive losses with obesity and recommend to their infertile patients with overweight to reduce it, then early diagnosis and correction of IR has not yet become the norm of examination of every infertile man with obesity, although it is IR that is the earliest (preclinical) and therefore reversible stage of type 2 diabetes mellitus, which can and should be actively detected in all men with infertility against the background of obesity. IR leads to glycolytic stress of the nerve endings, i.e., in fact, initiates metabolic urogenital neuropathy, leading to a violation of ejacular dynamics and fertile properties of the ejaculate.
Causes and mechanism of infertility development
Reducing testosterone levels (androgen deficiency) is increasingly seen today as a possible new and pathogenetically important component of MS in men, since it has been proven that the frequency and severity of androgen deficiency in men is in reliable feedback not only with the frequency and severity of obesity, but also insulin resistance and type 2 diabetes.
Not only obesity (BMI > 30), but even just excess weight (BMI = 25-29) in men significantly increase the frequency of infertility compared to men with a normal body mass index (BMI = 20-22.4). Obesity worsens the quality of the ejaculate by reducing its volume and increasing the frequency of sperm DNA damage. Type 2 diabetes mellitus - a frequent companion of obesity - can lead to the development of ejaculatory dysfunction, which can also cause a violation of the delivery of sperm into the female genital tract.

Recently, the oxidative theory of the pathogenesis of male infertility has become very popular, with metabolic syndrome playing a major role in it. The components of MS lead to an increase in free radicals of active oxygen in the ejaculate, followed by hyperperoxidation of sperm membranes and damage to their DNA.
Thus, the presence of MS in a man of any age with infertility is an indication not only to clarify the causes of hormonal metabolic disorders, but also to actively search for oxidative sperm stress.
Modern literary sources associate a decrease in reproductive potential in obese men with such pathophysiological phenomena as a deficiency of sex hormones (primarily testosterone), hormone D, endothelial dysfunction and a deficiency of regional circulation, including testicular blood flow, against the background of pronounced vasoconstriction due to a deficiency of nitric oxide (NO); excessive activity of the prooxidant blood system; excess of triglycerides and free fatty acids, which ultimately lead to a decrease in the number of sexually morphic cells, and permiosmosis.
According to the generally accepted point of view, oxidative stress of sperm develops when the dynamic balance between oxidants and antioxidants in the seminal plasma is disturbed, and its frequency in male infertility, according to various authors, reaches 30-80%. Hyperproduction of reactive oxygen species - free radicals - can be detected in many pathological conditions, both related to the reproductive system (local factors - inflammation of the genital appendage glands, varicocele, urogenital infections), and not directly related to it, which play the role of systemic mechanisms of oxidative stress of sperm (any psycho-emotional stress, diabetes type 2): obesity, systemic chronic inflammation, smoking, poor ecology, lifestyle and nutrition.
Thus, at present, the explanation of the influence of many negative pathophysiological mechanisms of obesity (systemic chronic inflammation, dyslipidemia, disorders of carbohydrate metabolism, androgen deficiency, fat lipotoxicity, etc.) on spermatogenesis is directly or indirectly associated with the theory of oxidative stress of spermatozoa, which they induce during the entire time while a man has obesity, the persistence and development of which they contribute to the progression of obesity in an infertile man.
Causes of male infertility: insulin resistance
Insulin resistance, or hyperinsulinemia, being a key pathogenetic factor of MS, is a complex of compensatory and adaptive reactions that develop against the background of obesity, often associated with androgen deficiency in men.
With the development and progression of obesity, the expression of the insulin receptor gene decreases sharply, which leads to a decrease in the density of receptors on the cell surface and the emergence of insulin resistance, and a simultaneous increase in the level of the main hormone of adipose tissue - leptin - destroys the functional connection between the pituitary gland and gonads, which is the pathogenetic basis for the formation and progression of androgenic deficiency in men simultaneously with the progression of obesity and IR.
Developing IR is accompanied by hyperinsulinemia, which in this case ensures the maintenance of the efficiency of carbohydrate metabolism, viability and cell division. IR is the earliest and therefore potentially reversible stage of type 2 diabetes, so its early detection in any somatic diseases in obese men is an important preventive measure against type 2 diabetes and and androgen deficiency.
Early diagnosis of IR is indicated for all men of reproductive age with obesity and any other components of MS, since male infertility (especially the so-called idiopathic) can be pathogenetically associated with IR, the mechanisms of which in this case can be reduced to the following:
Early disruption of the structure and function of nervous tissue (glycolysis stress), while initial damage is noted in the smallest peripheral nerve endings of the organs of the urogenital system (kidneys, penis, prostate gland, testicles) (the effect of induction and progression of urogenital metabolic neuropathy).
Neuropathy leads to systemic and local vasoconstrictor-type reactions and ends with the development of endothelial dysfunction due to a deficiency of the main vasodilator - nitric oxide (since 90% of nitric oxide synthesis occurs not in the endothelium, but in the terminals of the nerve endings of blood vessels).
Any neuropathy is associated with the activation of the lipid peroxidation system - systemic oxidative stress, which is a powerful damaging factor for testicular parenchyma, which ends with impaired spermatogenesis (infertility) and (or) steroidogenesis (androgenic deficiency). A variant of this systemic effect of IR is oxidative (oxidative) sperm stress.
IR and obesity, being key components of MS, initiate systemic chronic inflammation (cytokine cascade reactions), which are actively involved in the implementation of another mechanism of damaging action on testicular tissue (an analogue of oxidative stress) - renal lipotoxicity, leading to a violation of the DNA structure of sperm.
In addition, hyperinsulinemia leads to an increase in systemic sympathetic activity through impaired glucose metabolism in ventromedial hypothalamic neurons, which is accompanied by increased activity of a-adrenoreceptors of the urogenital tract (autonomous sympathetic hyperactivity, or neuropathy) and triggers systemic oxidative stress. M.Sankhla et al. (2012) in a survey of 120 men aged 17-26 years with obesity and infertility revealed a significant increase in the level of malondialdehyde (a marker of systemic oxidative stress) with an increase in BMI (p<0 div="nbsp=">>
Among the mechanisms of impaired fertility in patients with disorders of carbohydrate metabolism, some authors call the characteristic for this group of patients lesion of the appendages of the testicles, which can lead to impaired sperm transport, as well as urogenital neuropathy (glycolysis stress of neurons), oxidative stress, leading to damage to the nuclear and mitochondrial DNA of sperm and their increased immobilization, as well as NO deficiency due to androgenic insufficiency and neuropathy, since 90% of NO synthesized in the vascular wall is of neuronal origin.
Conclusion
Thus, infertile young men with obesity, in the absence of caution from the attending physician, there is always a danger of hypodiagnosis of the key component of MS - IR, which has a significant negative effect on spermatogenesis. From this point of view, it seems to us that the frequency of idiopathic infertility due to early detection of IR could be lower than it is commonly said. Idiopathic infertility today is most often infertility without a clear urological cause, since the problems of reproduction in our country are traditionally attributed to the competence of urologists. .
These are the imperatives of the twenty-first century – the age of pathogenetic and preventive medicine and interdisciplinary interactions. Therefore, a modern urologist from a surgeon should turn into a clinician and actively interact with related specialists (endocrinologists, therapists, neurologists).
Meridional tapping: The technique of emotional freedom
Key to the muscles of the cortex: lumbar muscle (psoas)
If this does not happen, then there is a high probability that in solving male reproductive problems in our country, the urologist will soon be a simple dispatcher who prescribes a couple exclusively referrals to reproductive clinics, since we are not able to stop the global epidemic of “diseases of civilization”, which today are the leading systemic pathophysiological initiators of oxidative sperm stress, clinically ending in male infertility. published
Author: Andrey Beloveskin
P.S. And remember, just by changing your consciousness – together we change the world!
Source: www.beloveshkin.com/2015/08/prichiny-muzhskogo-besplodiya-rezhim-deficita-leptin-insulin.html
Puff pastry pie pita with cheese and herbs — brilliant simplicity!
How to build an eco-house? Basic principles of green building