806
When insulin resistance is useful: from immunity to sleep
Accurate understanding of biological processes is very important for the selection of appropriate actions. Because many harmful manifestations of the disease is actually manifestations of the negative effect of the disease, but rather the body's attempt to deal with the problem.
So, fever enhances the fight against viruses and abuse of antipyretic can you get chronic infection, increase in heart rate may be an adaptive reaction during dehydration and so on. But very often adaptive, adaptive reaction can go very far and begin to create additional problems.
And here it is important to understand – where is the line between adaptation and pathology? I talk a lot about insulin resistance and emphasize both negative and positive aspects of the actions of the hormone insulin. Also, we often talk about insulin resistance, which is perceived as an absolute evil.
It is not so today we will talk about adaptive, adaptive properties of physiological insulin resistanceto gain a deeper understanding of this phenomenon and more precisely to work with him. At the end of the article I'll even tell people about the benefits of insulin resistance and how to benefit.
What is insulin resistance (insulin resistance)?
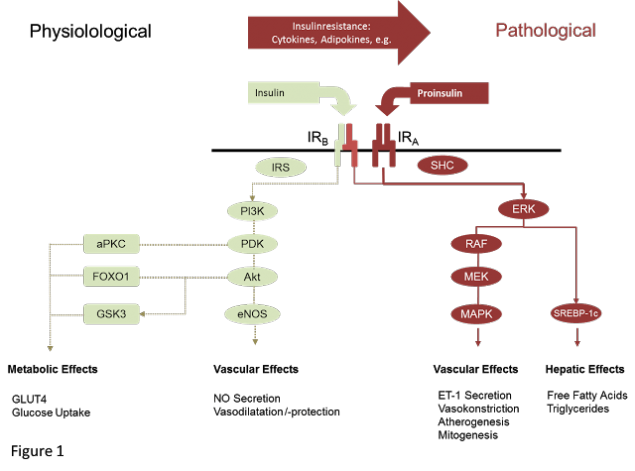
Insulin resistance (hereinafter IR) is an impaired metabolic response to insulin. Insulin resistance is a physiological condition in which cells (primarily liver, muscle, adipose tissue) do not respond to the normal actions of the hormone insulin.
The body produces insulin, but the cells in the body become resistant to insulin and cannot use it effectively. This concept applies to all the physiological effects of insulin, its effect on protein, fat metabolism, a state of vascular endothelium.
Resistance can develop as one of the effects of insulin independently of the other, and comprehensively. For a more accurate assessment of insulin resistance index HOMA. But unfortunately, insulinorezistentnost in most cases, is not recognized until the occurrence of metabolic disorders.
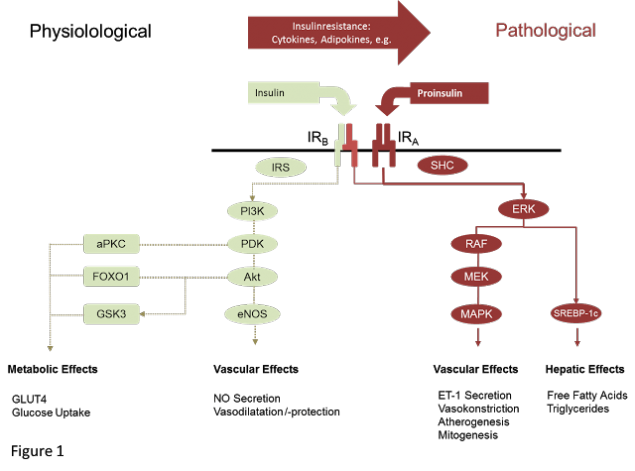
Yes, of course, that physiological (peripheral, muscle) insulin resistance is significantly different from the pathological (Central, hepatic).
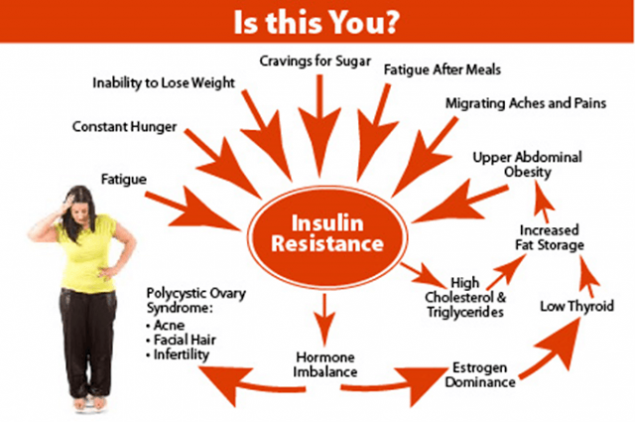
Physiological YR: puberty; pregnancy; night sleep; a diet rich in fat. Enhance IL-overeating, physical inactivity, stress, lack of sleep etc. In some cases, physiological insulin resistance can develop into pathological.
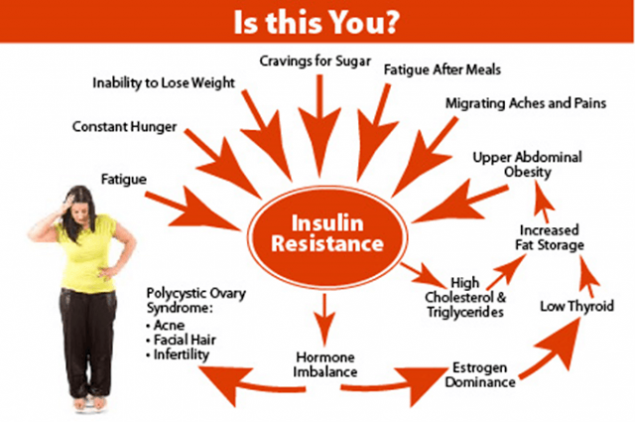
So, pregnant physiological insulin resistance develops into diabetes and weight gain, physiological insulin resistance in adolescent girls develops into the polycystic ovary syndrome, night physiological insulin resistance easily develops into obesity if you begin to eat later in the evenings.
Remember – physiological insulin resistance is not dangerous if you don't abuse calories. And if you do no exercise, then everything will be just fine.
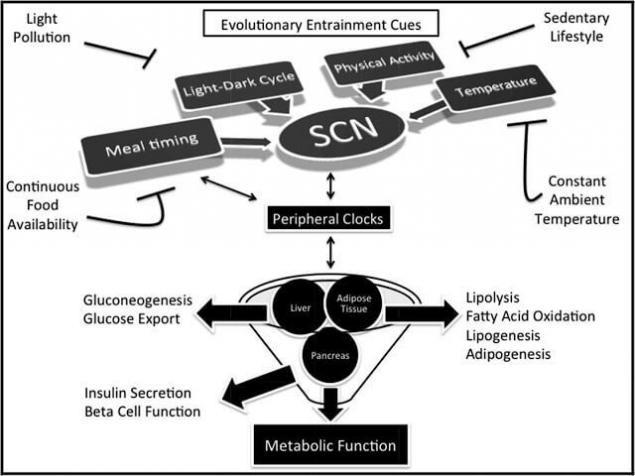
Insulin resistance and control metabolism.
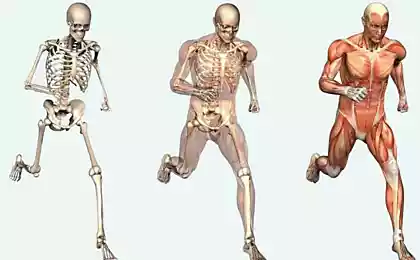
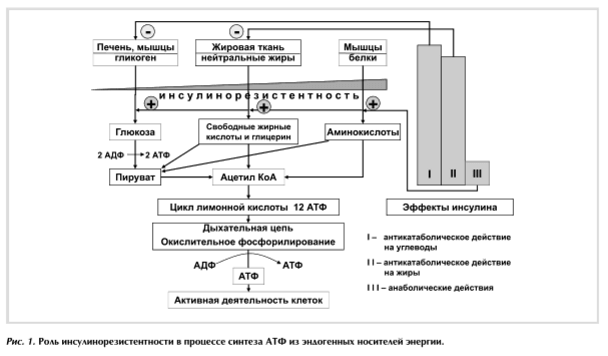
In the formation of energy used sequentially carbohydrates, fats and proteins. Such a sequence is strictly observed during the day and the dynamics of the processes of life throughout a person's life. To provide this sequence can insulin, since the tissues have different sensitivity to it.
Most sensitive to the anti-catabolic action of insulin, the glycogen of the liver, slightly less fatty tissue. Evidence that suppression of lipolysis by 50% required 10 mked/ml of insulin, and to suppress hepatic glucose production by 50% — 30 mked/ml of the hormone do not contradict this, because the production of glucose by the liver consists of glycogenolysis and gluconeogenesis.
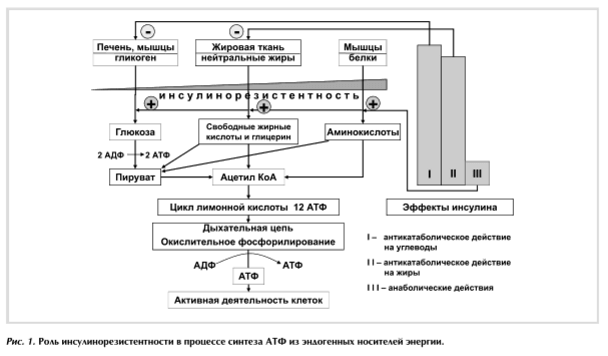
Mechanisms of IR can function efficiently and effectively.
With the effective way the body will use mainly carbohydrates and fats for the production of ATP (energy). In this case, the disruption in the body's system small. This method of energy production is observed in the adult healthy organism, which is at rest or normal activities. Under certain physiological conditions is quite is to increase ER, when significantly increases energy production in the target organ or in the organism as a whole, and amino acids appearing in the protein catabolism, used for the synthesis of energy, and in cosmetic purposes. So the mechanisms of IR in Feto-placental development, the newborn, the teenager, during physiological sleep, when muscle activity, benign and malignant tumors etc.
If inefficient way of functioning of the mechanisms of IR for production of ATP by endogenous proteins are involved that disrupt the system much more. However, the decrease of the anabolic effects of insulin, accompanied by violation of the phosphorylation of glucose, decreased energy production, decreased hypoglycemic effect of insulin, which leads to metabolic and functional disorders, which is most fully manifested by the development of diabetes mellitus 2 type (DM2). So the mechanisms of IR in hypertension, aging, obesity, pregnancy, endocrine pathology, etc.
The self-regulation system of the body performs a gradually increasing IR in the dynamics of development processes. She consistently releases from the depot glucose, derivatives of fats and amino acids (in that order). The actions of insulin directly or indirectly affect almost all body systems. Therefore, they are also involved in the regulation of metabolism, i.e., they are mechanisms of IR. The level of IR is the integrated indicator, where are existing between the numerous systems interconnection.
Insulin resistance is a historically established mechanism of adaptation of human organism to changing external conditions to maintain energy balance and normal functioning of all organs and systems.
A physiological condition predispose to IR: old age, pregnancy, night sleep, physical inactivity, puberty, obesity, infection, stress, starvation, uremia, liver cirrhosis, ketoacidosis, antibodies that block the receptors of insulin, endocrine diseases (Cushing's syndrome, acromegaly, pheochromocytoma, glucagonoma, thyrotoxicosis, hypothyroidism).
Diurnal, seasonal, age-related pregnancy, disease, fluctuations of food intake and energy expenditure require homeostatic versatility, including the ability to modify insulin sensitivity, which allows interstitial membrane to optimize a variable nutrient supply.
For example, in response to their short-term excess, skeletal and heart muscles become temporarily insulinorezistentne, physiological adaptation contributes to the redirection of excess nutrients into adipose tissue for storage. Found the dependence of the index of insulin resistance in healthy women from the phase of the menstrual cycle shows a decrease in folikulyarnogo phase correlated with reduced levels of progesterone in the physiology.
So now it is believed that insulin resistance allows us to more effectively store fat, which will be needed during periods of food scarcity. This property helps the body safely survive the famine. But modern humans through consumption of high-calorie and fatty foods developing obesity and metabolic syndrome.
According to the hypothesis of the "Thrifty genotype", put forward by V. Neel (1962), IR – fixed is an evolutionary survival mechanism in adverse conditions, when periods of starvation alternated with periods of abundance.
In modern conditions in the countries with a high level of life, and concomitant abundance, preserved in genetic memory mechanisms of IR continue to "work" on the accumulation of energythat leads to the development of abdominal obesity, dyslipidemia, hypertension, and finally type 2 diabetes.
During the famine of IR was formed to glucose from glycogenolysis, gluconeogenesis and lipolysis were sent in non-insulin dependent tissues (brain and heart) and was their supply of energy. This lasted until the next of abundance.
Originally, IR was seen as help a person to survive in unfavorable environmental conditions. I draw your attention that IR does not represent a threat to you, if you don't eat! We will return to this point. In the process of phylogenesis of this feature of metabolism has led to a significant prevalence of IR in society: it is revealed one in four healthy volunteers.
A scientific argument.
In September 2015 in Stockholm (Sweden) held international conference of endocrinologists "insulin resistance – benefit or harm?", where in the course of the discussion, E. Ferrannini and D. R. Matthews were considered two polar points of view on the issue of IR.
E. Ferrannini to the question, "insulin resistance is a benefit or harm?" said that it is always a harm. In support of his opinion he discussed the well-known data that we outlined earlier.
There is another, polar, previous, look at the problem of IR. His supporters D. R. Matthews, V. Neel, P. Poulsen, and M. DiPasquale do not deny the negative impact of IR that have been listed above, however, the special role they have to the mechanism of IR.
They believe that IR was originally developed as an adaptive, protective reaction of the body on action of pathological factors. Opponent the previous Rapporteur D. R. Matthews pointed to the fact that along with IR, there are insulinchuvstvitelnyh. While IR is in their "physiological limits", she is not a pathological process. D. R. Matthews points to a complex relationship between β-cells and insulin resistance: IR and dysfunction of β-cells, on the one hand, can lead to the development of type 2 diabetes, and with another – β-cells and insulin resistance can exist in a balanced way.
"IR is a physiological process, but it can become pathological (like any other physiological process) is influenced by genetic defect, drugs, overeating, etc. the Main reason for the switch IL in the pathological process that in the process of evolution has failed to find a balance between overeating and genetically determined ability of β-cells. To stay physiological process, it should be combined with exercise, a low calorie diet and a healthy lifestyle, "–says D. R. Matthews.
According to P. Poulsen et al (1999), in the development of IR along with the inheritance, a significant role for external factors (overeating, obesity, lack of exercise, chronic stress, hyperlipidemia).
M. DiPasquale in 2009 in the journal Body Building published an article entitled "Fat Confusion: Is Fat Bad For You?", where wrote about the fact that IR is good. Its presence contributes to a more rapid weight loss. Glucose the cell takes in insufficient quantity, so in order to insulin-dependent cells do not suffer from a lack of energy (as energy from gluconeogenesis and glycogenolysis is insufficient to cover all energy cells), they start to split FFA by β-oxidation, respectively fat mass decreases. Then IR will help to break down fats and oxidize FFA in the liver for energy. Thus, IL can even help you lose weight and soon I will tell you how to use this knowledge.
In March 2015, C. J. Nolan and co-authors published a work which questioned the dogma that insulin resistance (IR) is primarily harmful to the body and it must wage an irreconcilable struggle at any cost.
The authors recognize that IR is a physiological mechanism that protects critical tissue of the cardiovascular system from nutrient-induced injury. This, they explain a high risk subgroup of patients gaining weight, on the background of intensification of hypoglycemic therapy. It is argued that the desire to reduce plasma glucose levels, especially during intensive insulin therapy may harmful.
In large studies of patients with diabetes factory settings are that strict insulin therapy has not had a visible improvement. As the argument is formulated as: reduction of blood glucose, which occurs by overcoming IRA, supplying even more nutrients to an already overloaded tissue, which can paradoxically enhance metabolic damage in critical DanaH. Introduced the concept of "insulin-induced metabolic stress" in obese patients with diabetes mellitus type 2 (DM2) with different levels of metabolic control allows the most likely to explain the negative results of large clinical trials of T2DM.
To choose the correct answer requires a detailed analysis of the situation in which there is insulin resistance, although often it becomes a special challenge. In uncomplicated pregnancy, or in the development of short-term reactions "respiratory burst" leading to the elimination of bacterial infection, insulin resistance is a responsive, physiologically justified response. After childbirth or defeat the infection it goes away and does not require treatment.
Let us examine 5 physiological feeds and find out why insulinorezistentnost with them is absolutely fine and even great.
1. Night insulin resistance.
2. Puberty
3. Pregnancy
4. Low-carb food
5. Inflammation.
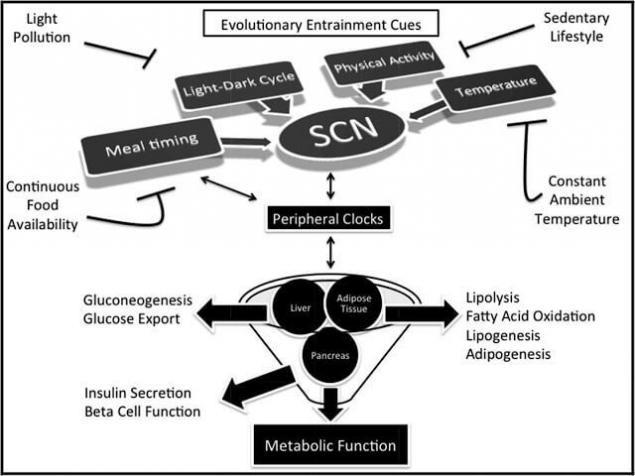
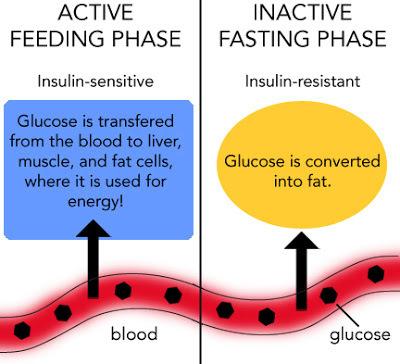
Night insulin resistance.
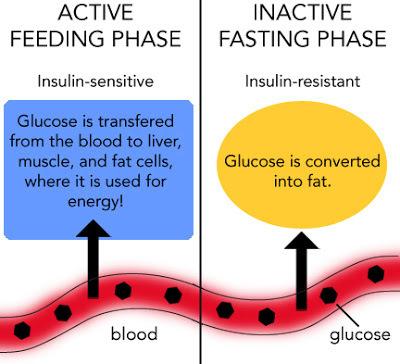
In the morning the insulin sensitivity is maximum and it crashes throughout the day. In the body there are two main ways of energy provision: "day" and "night".
When the "day" the way of energy main source of energy is glucose and, to a lesser extent fat.
At night, on the contrary, the body gets energy mainly from fatty acid that enters the blood during the breakdown of body fat.
But with obesity the daily switching mechanism of energy homeostasis is disturbed and the body goes mainly on fat way ensure.
The most important part of calories consumed in the morning, then they are absorbed on the background of increased insulin sensitivity.The food in the evening (when low sensitivity to insulin) leads to serious health problems.
Puberty and insulin resistance.
During the survey a total of 224 people aged 1 to 20 years, not obese, Laron et al found that the levels of insulin and C-peptide increases sharply at the onset of pubertyand, although glucose levels remained unchanged.
The maximum concentration of insulin on an empty stomach, often exceeding 75 mcmol/l, is achieved by the middle of the puberty, regardless of calendar age. After the onset of puberty the level of insulin is progressively reduced, reaching prepubertal values. These data confirm the assumption that puberty is accompanied by a physiological insulin resistance.
The opposite effects of two anabolic hormones (growth hormone GH and insulin) in the period of active growth seems paradoxical. However, Amiel et al demonstrated that insulin resistance is limited by the impact on glucose metabolism and does not affect the metabolism of amino acids. Thus compensatory hyperinsulinemia increases protein synthesis, stimulating growth.
Moreover, it is known that insulin is an important modulator of the actions of insulin-like growth factor 1 (IPP-1). IPFR-1, a structural analogue of proinsulin, mediates the growth-stimulating effect of GR. In addition to the main site of synthesis IPFR-1 — of the liver, many tissues also produce as this peptide and the receptor to it.
Since insulin exerts diverse metabolic effects, it sinhroniziruete the processes of growth and puberty with an optimal level of metabolism in the body. This adaptation is extremely important because on the one hand saves energy if there is insufficient food, and with another — to accelerate the maturation and fertility when a sufficient amount of food.
This theory may explain many clinical observations, such as: introduction G children with deficiency leads not only to stimulate growth but also to puberty. The fact that after the completion of puberty the levels of sex steroids remains high, whereas insulin resistance disappears, exclude sex hormones as a cause for development of insulin resistance.
Pregnancy and insulin resistance.
Glucose is the main source of energy for mother and fetus. The growth of the fetus needs more glucose, with consumption in the second half of pregnancy is ahead of its availability. Therefore, normal level of glucose in the blood of the fetus 10-20 mg/100 ml (0,6–1,1 mmol/l) was lower than that of the mother. (Physiological norm for pregnant women is 3.3 and 6.6 mmol/L.)
Noteworthy is the fact that in the period of maximum growth of the fetus in all pregnant developed physiological insulin resistance, which likely flows of glucose and forwarded from the bodies of the mother to the growing fetus.
This effect adjusts the placenta — the main source of secretion of TNF-α during pregnancy, especially in the second half. Approximately 94% of the placental TNF-α is released into the mother's bloodstream, and only 6% in the bloodstream of the fetus. Thus, high levels of TNF-α provides insulinorezistentnost maternal tissues.
After birth, its concentration sharply decreases rapidly, and in parallel restores insulin sensitivity. However, in pregnant women with overweight the contents of TNF-α significantly higher than in pregnant women with normal weight. Extremely fat women pregnancy often occurs with complications, and postpartum insulin sensitivity not only recovered, but also increases the risk of developing diabetes. However, with proper pregnancy adaptive insulin resistance, helps normal growth of the fetus.
Low carb fat diet.
Low-carb diet stimulates insulin resistance. This is a completely normal physiological response to limitation proceeds of carbohydrates with food, so as lowering insulin sensitivity improves fat burning. This restriction proceeds of carbohydrates reduces the production of insulin.
With a low level of insulin activates endocrine lipase (triglyceridemia). Adipose tissue breaks down and admits free fatty acids in the blood. These acids are mainly consumed by the muscle tissue and automatically call it insulin resistance.
This reaction is quite natural, since muscle tissue easily eats fats, leaving glucose for those tissues and organsthat really need it, for example, the brain. Nervous tissue different uses insulin to capture glucose, but never use grease, as it makes the muscle tissue and therefore, from the point of view of brain cells, physiological insulinrezistentnost is not a problem.
While muscles are in "refusal" glucose, any of its in the bloodstream, whether it is food or gluconeogenesis in the liver to quickly raise blood glucose levels. And it is quite normal if your way of eating is low in carbohydrates. It also means that you will fail the oral test glucosetolerance (OGTT) and the doctor hung a label on you diabetic.
In fact, even a single meal high in fat can lead to this, prolonging the physiological insulin resistance on the whole day. Common condition for OGTT is the intake of 150 grams of carbohydrates daily for three days before the test!!! An increased amount of free fatty acids induces physiological insulin resistance and elevated levels of tomakomai blood glucose. Easily switch to a more high carbohydrate food (in my case) runs normal pancreatic and muscle function.
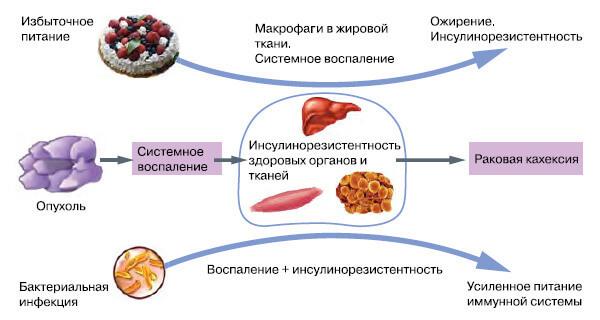
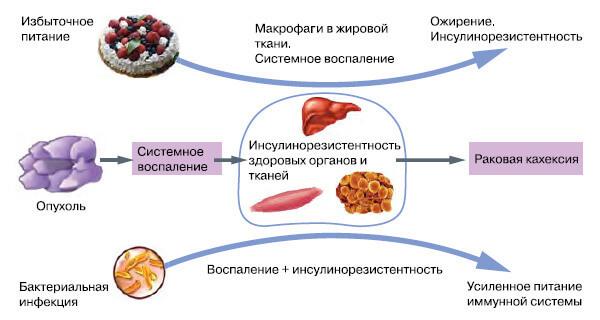
Inflammation and insulin resistance.
Inflammation is not a disease but a normal reaction, particularly a bacterial infection.The purpose of inflammation is to destroy bacteria through cytotoxic reactions "respiratory" or "oxygen explosion".
This name it received because of the cell-phagocytes that captured bacteria or products of their decay rapidly (explosively) increase the consumption of oxygen and glucose, which are involved in the formation of highly active radicals with antibacterial activity. For the implementation of the reaction of "respiratory explosion" a required fast delivery of large amounts of glucose to activated phagocytes.
Such a directed flow of the glucose is provided by the physiological mechanism of insulin resistance, which temporarily restricts the inflow of glucose into muscle and fat cells, directing it mainly in neutrophils and macrophages.
When inflammation distinguished inflammatory molecule e.g., TNF-α, which in high concentrations turns into an endotoxin, causing systemic inflammation, insulin resistance and long-term restriction of glucose in muscle, liver and adipose tissue.
Insulin resistance+overeating = trouble.
Physiological (peripheral muscle) andinsulinorezistentnost significantly different from pathological (Central, hepatic). In some cases, physiological insulin resistance can develop into pathological. So, pregnant physiological insulin resistance develops into diabetes and weight gain, physiological insulin resistance in adolescent girls develops into the polycystic ovary syndrome, night physiological insulin resistance easily develops into obesity if you begin to eat later in the evenings.
Remember – physiological insulin resistance is not dangerous if you don't abuse calories. And if you do not physical inactivity, that'll be just fine.
Here is an example. So, in 1992, Hales and Barker formulated the concept of the influence of environmental factors (in particular, undernutrition at an early age) on the development of diabetes mellitus type 2 in adults.
They found a correlation between low body weight at birth and the development of type 2 diabetes in men in England. Similar results were obtained on other populations and ethnic groups, the correlation has spread also to the previously described state of insulin resistance.
According to the hypothesis of the "Thrifty phenotype" malnutrition is getting to the fetus and newborn stress factor, which kompensiruet transition to a more efficient metabolism. Such adaptation is designed to prepare the organism to survive in conditions of lack of nutrients.
One of the changes is the development of insulin resistance in muscle and adipose tissues, creating the relative protection of the growth and activity of the brain. Adaptive metabolic changes lose their protective role, when in the postnatal period the baby receives nutrients in excess amounts, which leads to the development of obesity and diabetes.
Ie, if kids ate a little, then diabetes would have not happened! But if their mothers ate normally during pregnancy, before the excess nutrients wouldn't hurt their children!
Conclusion.
Thus, insulin resistance is a physiological process and acts as a compensatory reaction, often aimed at protecting the body from various stressors. However, the pri the presence of hereditary predisposition and exposure to risk factors, IR becomes abnormal orientation, contributes to the development of type 2 diabetes, hypertension, dyslipidemia, PCOS and other severe diseases.
Effective natural remedy against viruses, bacteria, yeast and fungiIMPORTANT! It is necessary to know in order not to die from breast cancer
But how not to cross that thin line between physiological and pathological process, and most importantly, how to manage IR? This is a complex question and often individual. But one hint I'll give: for the safe flow of IR it is important to limit calorie, especially carbohydrates. This will bring all the side effects of IR to a minimum.
IR occurs for a kind of "protection" of tissues from glucose, so a moderate restriction of food and increase in physical activity allows you to effectively cope with AndR. published
Sources:
www.science-education.ru/ru/article/view?id=24290
Wallace TM, Matthews Dr. The assessment of insulin resistance in man. Diabet Med 19, 527-534
Different faces of insulin resistance Shvartsburg P. M.,"Chemistry and life" №7, 2013
xn--80aanlliihhlpcdkejz4b9g4b.xn--p1ai/%D0%B8%D0%BD%D1%81%D1%83%D0%BB%D0%B8%D0%BD%D0%BE%D1%80%D0%B5%D0%B7%D0%B8%D1%81%D1%82%D0%B5%D0%BD%D1%82%D0%BD%D0%BE%D1%81%D1%82%D1%8C/
cyberleninka.ru/article/n/insulinorezistentnost-i-regulyatsiya-metabolizma
medi.ru/info/11288/
www.ncbi.nlm.nih.gov/pmc/articles/PMC3595381/
www.med2000.ru/perevod/perevod13.htm
Author: Andrey Blueskin
Source: www.beloveshkin.com/2017/01/kogda-insulinorezistentnost-byvaet-polezna.html
So, fever enhances the fight against viruses and abuse of antipyretic can you get chronic infection, increase in heart rate may be an adaptive reaction during dehydration and so on. But very often adaptive, adaptive reaction can go very far and begin to create additional problems.
And here it is important to understand – where is the line between adaptation and pathology? I talk a lot about insulin resistance and emphasize both negative and positive aspects of the actions of the hormone insulin. Also, we often talk about insulin resistance, which is perceived as an absolute evil.
It is not so today we will talk about adaptive, adaptive properties of physiological insulin resistanceto gain a deeper understanding of this phenomenon and more precisely to work with him. At the end of the article I'll even tell people about the benefits of insulin resistance and how to benefit.
What is insulin resistance (insulin resistance)?
Insulin resistance (hereinafter IR) is an impaired metabolic response to insulin. Insulin resistance is a physiological condition in which cells (primarily liver, muscle, adipose tissue) do not respond to the normal actions of the hormone insulin.
The body produces insulin, but the cells in the body become resistant to insulin and cannot use it effectively. This concept applies to all the physiological effects of insulin, its effect on protein, fat metabolism, a state of vascular endothelium.
Resistance can develop as one of the effects of insulin independently of the other, and comprehensively. For a more accurate assessment of insulin resistance index HOMA. But unfortunately, insulinorezistentnost in most cases, is not recognized until the occurrence of metabolic disorders.
Yes, of course, that physiological (peripheral, muscle) insulin resistance is significantly different from the pathological (Central, hepatic).
Physiological YR: puberty; pregnancy; night sleep; a diet rich in fat. Enhance IL-overeating, physical inactivity, stress, lack of sleep etc. In some cases, physiological insulin resistance can develop into pathological.
So, pregnant physiological insulin resistance develops into diabetes and weight gain, physiological insulin resistance in adolescent girls develops into the polycystic ovary syndrome, night physiological insulin resistance easily develops into obesity if you begin to eat later in the evenings.
Remember – physiological insulin resistance is not dangerous if you don't abuse calories. And if you do no exercise, then everything will be just fine.
Insulin resistance and control metabolism.
In the formation of energy used sequentially carbohydrates, fats and proteins. Such a sequence is strictly observed during the day and the dynamics of the processes of life throughout a person's life. To provide this sequence can insulin, since the tissues have different sensitivity to it.
Most sensitive to the anti-catabolic action of insulin, the glycogen of the liver, slightly less fatty tissue. Evidence that suppression of lipolysis by 50% required 10 mked/ml of insulin, and to suppress hepatic glucose production by 50% — 30 mked/ml of the hormone do not contradict this, because the production of glucose by the liver consists of glycogenolysis and gluconeogenesis.
Mechanisms of IR can function efficiently and effectively.
With the effective way the body will use mainly carbohydrates and fats for the production of ATP (energy). In this case, the disruption in the body's system small. This method of energy production is observed in the adult healthy organism, which is at rest or normal activities. Under certain physiological conditions is quite is to increase ER, when significantly increases energy production in the target organ or in the organism as a whole, and amino acids appearing in the protein catabolism, used for the synthesis of energy, and in cosmetic purposes. So the mechanisms of IR in Feto-placental development, the newborn, the teenager, during physiological sleep, when muscle activity, benign and malignant tumors etc.
If inefficient way of functioning of the mechanisms of IR for production of ATP by endogenous proteins are involved that disrupt the system much more. However, the decrease of the anabolic effects of insulin, accompanied by violation of the phosphorylation of glucose, decreased energy production, decreased hypoglycemic effect of insulin, which leads to metabolic and functional disorders, which is most fully manifested by the development of diabetes mellitus 2 type (DM2). So the mechanisms of IR in hypertension, aging, obesity, pregnancy, endocrine pathology, etc.
The self-regulation system of the body performs a gradually increasing IR in the dynamics of development processes. She consistently releases from the depot glucose, derivatives of fats and amino acids (in that order). The actions of insulin directly or indirectly affect almost all body systems. Therefore, they are also involved in the regulation of metabolism, i.e., they are mechanisms of IR. The level of IR is the integrated indicator, where are existing between the numerous systems interconnection.
Insulin resistance is a historically established mechanism of adaptation of human organism to changing external conditions to maintain energy balance and normal functioning of all organs and systems.
A physiological condition predispose to IR: old age, pregnancy, night sleep, physical inactivity, puberty, obesity, infection, stress, starvation, uremia, liver cirrhosis, ketoacidosis, antibodies that block the receptors of insulin, endocrine diseases (Cushing's syndrome, acromegaly, pheochromocytoma, glucagonoma, thyrotoxicosis, hypothyroidism).
Diurnal, seasonal, age-related pregnancy, disease, fluctuations of food intake and energy expenditure require homeostatic versatility, including the ability to modify insulin sensitivity, which allows interstitial membrane to optimize a variable nutrient supply.
For example, in response to their short-term excess, skeletal and heart muscles become temporarily insulinorezistentne, physiological adaptation contributes to the redirection of excess nutrients into adipose tissue for storage. Found the dependence of the index of insulin resistance in healthy women from the phase of the menstrual cycle shows a decrease in folikulyarnogo phase correlated with reduced levels of progesterone in the physiology.
So now it is believed that insulin resistance allows us to more effectively store fat, which will be needed during periods of food scarcity. This property helps the body safely survive the famine. But modern humans through consumption of high-calorie and fatty foods developing obesity and metabolic syndrome.
According to the hypothesis of the "Thrifty genotype", put forward by V. Neel (1962), IR – fixed is an evolutionary survival mechanism in adverse conditions, when periods of starvation alternated with periods of abundance.
In modern conditions in the countries with a high level of life, and concomitant abundance, preserved in genetic memory mechanisms of IR continue to "work" on the accumulation of energythat leads to the development of abdominal obesity, dyslipidemia, hypertension, and finally type 2 diabetes.
During the famine of IR was formed to glucose from glycogenolysis, gluconeogenesis and lipolysis were sent in non-insulin dependent tissues (brain and heart) and was their supply of energy. This lasted until the next of abundance.
Originally, IR was seen as help a person to survive in unfavorable environmental conditions. I draw your attention that IR does not represent a threat to you, if you don't eat! We will return to this point. In the process of phylogenesis of this feature of metabolism has led to a significant prevalence of IR in society: it is revealed one in four healthy volunteers.
A scientific argument.
In September 2015 in Stockholm (Sweden) held international conference of endocrinologists "insulin resistance – benefit or harm?", where in the course of the discussion, E. Ferrannini and D. R. Matthews were considered two polar points of view on the issue of IR.
E. Ferrannini to the question, "insulin resistance is a benefit or harm?" said that it is always a harm. In support of his opinion he discussed the well-known data that we outlined earlier.
There is another, polar, previous, look at the problem of IR. His supporters D. R. Matthews, V. Neel, P. Poulsen, and M. DiPasquale do not deny the negative impact of IR that have been listed above, however, the special role they have to the mechanism of IR.
They believe that IR was originally developed as an adaptive, protective reaction of the body on action of pathological factors. Opponent the previous Rapporteur D. R. Matthews pointed to the fact that along with IR, there are insulinchuvstvitelnyh. While IR is in their "physiological limits", she is not a pathological process. D. R. Matthews points to a complex relationship between β-cells and insulin resistance: IR and dysfunction of β-cells, on the one hand, can lead to the development of type 2 diabetes, and with another – β-cells and insulin resistance can exist in a balanced way.
"IR is a physiological process, but it can become pathological (like any other physiological process) is influenced by genetic defect, drugs, overeating, etc. the Main reason for the switch IL in the pathological process that in the process of evolution has failed to find a balance between overeating and genetically determined ability of β-cells. To stay physiological process, it should be combined with exercise, a low calorie diet and a healthy lifestyle, "–says D. R. Matthews.
According to P. Poulsen et al (1999), in the development of IR along with the inheritance, a significant role for external factors (overeating, obesity, lack of exercise, chronic stress, hyperlipidemia).
M. DiPasquale in 2009 in the journal Body Building published an article entitled "Fat Confusion: Is Fat Bad For You?", where wrote about the fact that IR is good. Its presence contributes to a more rapid weight loss. Glucose the cell takes in insufficient quantity, so in order to insulin-dependent cells do not suffer from a lack of energy (as energy from gluconeogenesis and glycogenolysis is insufficient to cover all energy cells), they start to split FFA by β-oxidation, respectively fat mass decreases. Then IR will help to break down fats and oxidize FFA in the liver for energy. Thus, IL can even help you lose weight and soon I will tell you how to use this knowledge.
In March 2015, C. J. Nolan and co-authors published a work which questioned the dogma that insulin resistance (IR) is primarily harmful to the body and it must wage an irreconcilable struggle at any cost.
The authors recognize that IR is a physiological mechanism that protects critical tissue of the cardiovascular system from nutrient-induced injury. This, they explain a high risk subgroup of patients gaining weight, on the background of intensification of hypoglycemic therapy. It is argued that the desire to reduce plasma glucose levels, especially during intensive insulin therapy may harmful.
In large studies of patients with diabetes factory settings are that strict insulin therapy has not had a visible improvement. As the argument is formulated as: reduction of blood glucose, which occurs by overcoming IRA, supplying even more nutrients to an already overloaded tissue, which can paradoxically enhance metabolic damage in critical DanaH. Introduced the concept of "insulin-induced metabolic stress" in obese patients with diabetes mellitus type 2 (DM2) with different levels of metabolic control allows the most likely to explain the negative results of large clinical trials of T2DM.
To choose the correct answer requires a detailed analysis of the situation in which there is insulin resistance, although often it becomes a special challenge. In uncomplicated pregnancy, or in the development of short-term reactions "respiratory burst" leading to the elimination of bacterial infection, insulin resistance is a responsive, physiologically justified response. After childbirth or defeat the infection it goes away and does not require treatment.
Let us examine 5 physiological feeds and find out why insulinorezistentnost with them is absolutely fine and even great.
1. Night insulin resistance.
2. Puberty
3. Pregnancy
4. Low-carb food
5. Inflammation.
Night insulin resistance.
In the morning the insulin sensitivity is maximum and it crashes throughout the day. In the body there are two main ways of energy provision: "day" and "night".
When the "day" the way of energy main source of energy is glucose and, to a lesser extent fat.
At night, on the contrary, the body gets energy mainly from fatty acid that enters the blood during the breakdown of body fat.
But with obesity the daily switching mechanism of energy homeostasis is disturbed and the body goes mainly on fat way ensure.
The most important part of calories consumed in the morning, then they are absorbed on the background of increased insulin sensitivity.The food in the evening (when low sensitivity to insulin) leads to serious health problems.
Puberty and insulin resistance.
During the survey a total of 224 people aged 1 to 20 years, not obese, Laron et al found that the levels of insulin and C-peptide increases sharply at the onset of pubertyand, although glucose levels remained unchanged.
The maximum concentration of insulin on an empty stomach, often exceeding 75 mcmol/l, is achieved by the middle of the puberty, regardless of calendar age. After the onset of puberty the level of insulin is progressively reduced, reaching prepubertal values. These data confirm the assumption that puberty is accompanied by a physiological insulin resistance.
The opposite effects of two anabolic hormones (growth hormone GH and insulin) in the period of active growth seems paradoxical. However, Amiel et al demonstrated that insulin resistance is limited by the impact on glucose metabolism and does not affect the metabolism of amino acids. Thus compensatory hyperinsulinemia increases protein synthesis, stimulating growth.
Moreover, it is known that insulin is an important modulator of the actions of insulin-like growth factor 1 (IPP-1). IPFR-1, a structural analogue of proinsulin, mediates the growth-stimulating effect of GR. In addition to the main site of synthesis IPFR-1 — of the liver, many tissues also produce as this peptide and the receptor to it.
Since insulin exerts diverse metabolic effects, it sinhroniziruete the processes of growth and puberty with an optimal level of metabolism in the body. This adaptation is extremely important because on the one hand saves energy if there is insufficient food, and with another — to accelerate the maturation and fertility when a sufficient amount of food.
This theory may explain many clinical observations, such as: introduction G children with deficiency leads not only to stimulate growth but also to puberty. The fact that after the completion of puberty the levels of sex steroids remains high, whereas insulin resistance disappears, exclude sex hormones as a cause for development of insulin resistance.
Pregnancy and insulin resistance.
Glucose is the main source of energy for mother and fetus. The growth of the fetus needs more glucose, with consumption in the second half of pregnancy is ahead of its availability. Therefore, normal level of glucose in the blood of the fetus 10-20 mg/100 ml (0,6–1,1 mmol/l) was lower than that of the mother. (Physiological norm for pregnant women is 3.3 and 6.6 mmol/L.)
Noteworthy is the fact that in the period of maximum growth of the fetus in all pregnant developed physiological insulin resistance, which likely flows of glucose and forwarded from the bodies of the mother to the growing fetus.
This effect adjusts the placenta — the main source of secretion of TNF-α during pregnancy, especially in the second half. Approximately 94% of the placental TNF-α is released into the mother's bloodstream, and only 6% in the bloodstream of the fetus. Thus, high levels of TNF-α provides insulinorezistentnost maternal tissues.
After birth, its concentration sharply decreases rapidly, and in parallel restores insulin sensitivity. However, in pregnant women with overweight the contents of TNF-α significantly higher than in pregnant women with normal weight. Extremely fat women pregnancy often occurs with complications, and postpartum insulin sensitivity not only recovered, but also increases the risk of developing diabetes. However, with proper pregnancy adaptive insulin resistance, helps normal growth of the fetus.
Low carb fat diet.
Low-carb diet stimulates insulin resistance. This is a completely normal physiological response to limitation proceeds of carbohydrates with food, so as lowering insulin sensitivity improves fat burning. This restriction proceeds of carbohydrates reduces the production of insulin.
With a low level of insulin activates endocrine lipase (triglyceridemia). Adipose tissue breaks down and admits free fatty acids in the blood. These acids are mainly consumed by the muscle tissue and automatically call it insulin resistance.
This reaction is quite natural, since muscle tissue easily eats fats, leaving glucose for those tissues and organsthat really need it, for example, the brain. Nervous tissue different uses insulin to capture glucose, but never use grease, as it makes the muscle tissue and therefore, from the point of view of brain cells, physiological insulinrezistentnost is not a problem.
While muscles are in "refusal" glucose, any of its in the bloodstream, whether it is food or gluconeogenesis in the liver to quickly raise blood glucose levels. And it is quite normal if your way of eating is low in carbohydrates. It also means that you will fail the oral test glucosetolerance (OGTT) and the doctor hung a label on you diabetic.
In fact, even a single meal high in fat can lead to this, prolonging the physiological insulin resistance on the whole day. Common condition for OGTT is the intake of 150 grams of carbohydrates daily for three days before the test!!! An increased amount of free fatty acids induces physiological insulin resistance and elevated levels of tomakomai blood glucose. Easily switch to a more high carbohydrate food (in my case) runs normal pancreatic and muscle function.
Inflammation and insulin resistance.
Inflammation is not a disease but a normal reaction, particularly a bacterial infection.The purpose of inflammation is to destroy bacteria through cytotoxic reactions "respiratory" or "oxygen explosion".
This name it received because of the cell-phagocytes that captured bacteria or products of their decay rapidly (explosively) increase the consumption of oxygen and glucose, which are involved in the formation of highly active radicals with antibacterial activity. For the implementation of the reaction of "respiratory explosion" a required fast delivery of large amounts of glucose to activated phagocytes.
Such a directed flow of the glucose is provided by the physiological mechanism of insulin resistance, which temporarily restricts the inflow of glucose into muscle and fat cells, directing it mainly in neutrophils and macrophages.
When inflammation distinguished inflammatory molecule e.g., TNF-α, which in high concentrations turns into an endotoxin, causing systemic inflammation, insulin resistance and long-term restriction of glucose in muscle, liver and adipose tissue.
Insulin resistance+overeating = trouble.
Physiological (peripheral muscle) andinsulinorezistentnost significantly different from pathological (Central, hepatic). In some cases, physiological insulin resistance can develop into pathological. So, pregnant physiological insulin resistance develops into diabetes and weight gain, physiological insulin resistance in adolescent girls develops into the polycystic ovary syndrome, night physiological insulin resistance easily develops into obesity if you begin to eat later in the evenings.
Remember – physiological insulin resistance is not dangerous if you don't abuse calories. And if you do not physical inactivity, that'll be just fine.
Here is an example. So, in 1992, Hales and Barker formulated the concept of the influence of environmental factors (in particular, undernutrition at an early age) on the development of diabetes mellitus type 2 in adults.
They found a correlation between low body weight at birth and the development of type 2 diabetes in men in England. Similar results were obtained on other populations and ethnic groups, the correlation has spread also to the previously described state of insulin resistance.
According to the hypothesis of the "Thrifty phenotype" malnutrition is getting to the fetus and newborn stress factor, which kompensiruet transition to a more efficient metabolism. Such adaptation is designed to prepare the organism to survive in conditions of lack of nutrients.
One of the changes is the development of insulin resistance in muscle and adipose tissues, creating the relative protection of the growth and activity of the brain. Adaptive metabolic changes lose their protective role, when in the postnatal period the baby receives nutrients in excess amounts, which leads to the development of obesity and diabetes.
Ie, if kids ate a little, then diabetes would have not happened! But if their mothers ate normally during pregnancy, before the excess nutrients wouldn't hurt their children!
Conclusion.
Thus, insulin resistance is a physiological process and acts as a compensatory reaction, often aimed at protecting the body from various stressors. However, the pri the presence of hereditary predisposition and exposure to risk factors, IR becomes abnormal orientation, contributes to the development of type 2 diabetes, hypertension, dyslipidemia, PCOS and other severe diseases.
Effective natural remedy against viruses, bacteria, yeast and fungiIMPORTANT! It is necessary to know in order not to die from breast cancer
But how not to cross that thin line between physiological and pathological process, and most importantly, how to manage IR? This is a complex question and often individual. But one hint I'll give: for the safe flow of IR it is important to limit calorie, especially carbohydrates. This will bring all the side effects of IR to a minimum.
IR occurs for a kind of "protection" of tissues from glucose, so a moderate restriction of food and increase in physical activity allows you to effectively cope with AndR. published
Sources:
www.science-education.ru/ru/article/view?id=24290
Wallace TM, Matthews Dr. The assessment of insulin resistance in man. Diabet Med 19, 527-534
Different faces of insulin resistance Shvartsburg P. M.,"Chemistry and life" №7, 2013
xn--80aanlliihhlpcdkejz4b9g4b.xn--p1ai/%D0%B8%D0%BD%D1%81%D1%83%D0%BB%D0%B8%D0%BD%D0%BE%D1%80%D0%B5%D0%B7%D0%B8%D1%81%D1%82%D0%B5%D0%BD%D1%82%D0%BD%D0%BE%D1%81%D1%82%D1%8C/
cyberleninka.ru/article/n/insulinorezistentnost-i-regulyatsiya-metabolizma
medi.ru/info/11288/
www.ncbi.nlm.nih.gov/pmc/articles/PMC3595381/
www.med2000.ru/perevod/perevod13.htm
Author: Andrey Blueskin
Source: www.beloveshkin.com/2017/01/kogda-insulinorezistentnost-byvaet-polezna.html