283
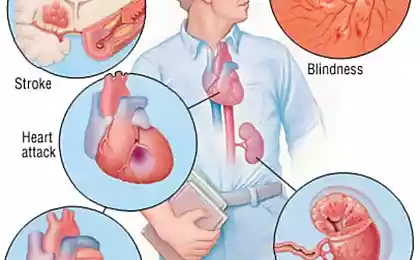
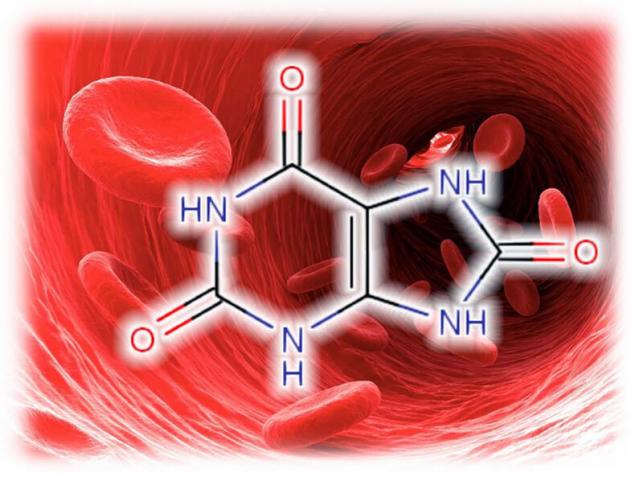
High levels of uric acid are a powerful risk factor for obesity, senile dementia and more!
Asymptomatic high levels of uric acid is a powerful risk factor for cardiovascular disease, obesity, atherosclerosis, senile dementia, impotence, etc.Normal MK levels are 6.5–7 mg/dL in men and 6–6.5 mg/dL in women.
Concentrations of 5.75 mg/dL or higher for men and 4.8 mg/dL or higher for women were classified as “high normal,” meaning a certain health effect. Uric acid is elevated if its level is more than 7.0 mg / dL and is associated with an increased risk of developing gout or kidney stones.
Elevated uric acid levels
A new wave of interest in uric acid is associated with an understanding of the role of asymptomatic hyperuricemia (defined most commonly as an increase in plasma uric acid levels of 7.0 mg/dL) as a powerful, independent and modifiable risk factor for cardiovascular disease and mortality, based on data from numerous epidemiological and prospective studies.
The most common causes affecting uric acid levels are obesity, insulin resistance, metabolic syndrome, arterial hypertension, use of diuretics and low doses of acetylsalicylic acid, excessive alcohol consumption, old age, kidney failure. Among them, the leading metabolic syndrome and its components. Alcohol, impaired renal function and obesity are also associated with higher levels of uric acid.
0. Asymptomatic increase in uric acid levels.
According to the recommendations of the EULAR (European Antirheumatic League), hyperuricemia (GU) is considered an increase in uric acid (MC) of blood serum above 360 μmol / l. It often happens that you have an elevated level of uric acid, but there is no disease, this condition happens according to a number of estimates, in Belarus and the Russian Federation, one in five.
According to more modest estimates, 5–8% of the population have an asymptomatic increase in the level of MK, of which only 5–20% develop gout Over the period from 1950 to 1980 in the population, the average serum MK level increased from 5 to 6 mg / dl.
Currently, the role of hyperuricemia as an independent predictor of cardiovascular morbidity and mortality in patients with coronary heart disease, chronic and acute heart failure, arterial hypertension and prehypertension and metabolic syndrome has been proven.
Nowadays, the question becomes more and more relevant: how “harmless” is an asymptomatic increase in uric acid levels? Read about that below.
1. Linking elevated uric acid levels to insulin resistance and obesity
An increase in uric acid, along with an increase in low-density lipoproteins, is considered part of insulin resistance syndrome, which leads to cardiovascular morbidity. Insulin resistance and hyperinsulinemia can reduce renal excretion of uric acid regardless of obesity and kidney function.
It is likely that insulin increases sodium tubular reabsorption, which is accompanied by an increase in uric acid reabsorption. Insulin resistance links hypertension, hypertriglyceridemia and hyperuricemia.
However, urinary is associated with triglycerides regardless of fasting insulin levels and obesity, showing that the mechanism underlying this association only partially relates to insulin resistance and obesity.
Selective insulin resistance is characteristic of patients with arterial hypertension, and insulin has a strong sodium retention effect, which is accompanied by a decrease in renal excretion of uric acid.
Hyperinsulinemia is also able to increase the activity of the sympathetic nervous system, which can contribute to an increase in uric acid in the blood. The view that hyperuricemia may be an indicator of insulin resistance was recently confirmed by an 8-year study proving a link between UMC and insulin resistance.
Thus, hyperuricemia in patients with arterial hypertension may indicate insulin resistance, which is definitely associated with increased cardiovascular morbidity.

Uric acid increased in abdominal obesity
Elevated levels of uric acid are obviously also associated with renal vascular resistance and have an inverse dependence on renal blood flow. Uric acid levels correlate with excretion of albumins in the urine, which are precursors to the development of nephrosclerosis, and a violation of renal hemodynamics precedes impaired uric acid metabolism in patients with nephropathy. Thus, hyperuricemia in patients with arterial hypertension most likely reflects a violation of renal hemodynamics, this is a good prognostic factor.
Many studies have found that urinary levels are associated with hyperlipidemia, particularly hypertriglyceridemia. A stronger association was found with triglycerides rather than cholesterol, leading to the suggestion that triglycerides are an intermediate link between increased uric acid and increased cholesterol. There was a weak association between uric acid levels and high-density lipoproteins.
2. The connection of uric acid with atherosclerosis.
Atherosclerosis is observed in birds, while being usually asymptomatic. Birds, like primates, eat a lot of fruit and secrete uric acid. Considering models of atherosclerosis in animals that have a different metabolism often yields potentially incorrect results. For example, the famous cholesterol rabbit is often not applicable to humans at all.
Uric acid is a pro-inflammatory substance in relation to the cardiovascular system, stimulating the release of pro-inflammatory cytokines. It is suggested that there are several potential mechanisms by which uric acid may play a pathogenetic role in the development of cardiovascular morbidity or, conversely, affect clinical manifestations in patients with established atherosclerosis, but none of them have yet been confirmed.
Obviously, elevated uric acid levels enhance the oxidation of low-density lipoproteins and promote lipid peroxygenation, and are also associated with increased production of free oxygen radicals. Oxidant stress and increased oxygenation of low-density lipoproteins in the artery wall may play a role in the progression of atherosclerosis. Uric acid may be involved in platelet adhesion and aggregation. This gave rise to the hypothesis that hyperuricemia increases the risk of coronary thrombosis in patients with already existing coronary diseases.
It is assumed that the increase in uric acid reflects damage to the endothelium. Endothelial dysfunction, manifested by a decrease in endothelium-dependent vascular relaxation as a result of the action of NO, is common in patients with diabetes and arterial hypertension and plays a role in the development of atherosclerosis.
In endothelial cells, xanthine oxide is present, which is a generator of free oxygen radicals. Uric acid and xanthine oxide are elevated and are determined in much greater concentrations in vessels affected by atherosclerosis than in healthy vascular tissue. If this mechanism is correct, then an increase in uric acid may be an accurate marker of a biological phenomenon closely associated with the progression of atherosclerosis, without directly causing the development of the process of vascular damage in which xanthine oxide may be responsible.

In turn, with constant hyperuricemia, the development of arterial hypertension is associated with the development of preglomerular arteriopathy and tubulointerstitial lesion. An increase in uric acid levels stimulates the activation of the renin-angiotensin system and exacerbates endothelial dysfunction.
In addition, under the conditions of ischemia, the enzyme xanthine oxyreductase is converted to xanthine oxidase, which leads to a change in xanthine metabolism, the conversion of uric acid from an antioxidant to a prooxidant and the stimulation of oxidative stress. Hyperuricemia leads to endothelial dysfunction by inhibiting NO synthesis. This effect of uric acid is due to its prooxidant properties under conditions of altered metabolism.
Uric acid also stimulates the proliferation of smooth muscle cells of blood vessels by activating growth factors, vasoconstrictor and pro-inflammatory molecules. Thus, uric acid is not only a marker, but also an active component of the development of hypertension.
However, most importantly, in the group of patients in whom thiazide diuretics led to an increase in MK, the number of cardiovascular events was 42% higher than in the group of patients who did not have an increase in MK.
The link between hyperuricemia (increased levels of uric acid) and the risk of cardiovascular disease has been established in large epidemiological studies. The relationship of high levels of uric acid with arterial hypertension, diabetes, insulin resistance, obesity and cardiovascular diseases caused by atherosclerosis has been proved.
The National Health and Nutrition Examination Survey (NHANES I) found an independent link between hyperuricemia and increased cardiovascular mortality. As MK levels increased, the risk of death from CHD increased by 77% in men and 300% in women. An increase in MK concentration of 1 mg/dL (59.5 μmol/L) was associated with a significant increase in mortality among both men and women.
A 12-year study (PIUMA), involving more than 1,500 previously untreated patients with hypertension, also demonstrated that serum levels are a strong predictor of cardiovascular morbidity and mortality.
A study of patients with type 2 diabetes showed a significant increase in the frequency of stroke with an increase in uric acid levels. The association remained significant even after other cardiovascular risk factors were excluded. Meanwhile, the results of the Framingham study did not reveal a significant association between uric acid levels and cardiovascular morbidity.
Hyperuricemia has been found in nearly 90% of adolescents with newly diagnosed hypertension. The results of studies indicate that the correction of hieruricemia can prevent the development of cardiovascular disasters.
So what to do with an asymptomatic increase in uric acid?
It has been shown that not only sodium monourate crystals, but also soluble uric acid in asymptomatic GI can lead to an increase in the level of inflammatory mediators and induce the proliferation of vascular smooth muscle cells in vitro. Many of these “pro-inflammatory” mediators are fundamental in the pathogenesis of atherosclerotic vascular damage and its complications. Therefore, you should slightly change the diet, about this in the next article.
Researchers from Johns Hopkins Medical University (Baltimore, Maryland, USA) found that individuals with “high normal” levels of uric acid have a volume of hyperintensive white matter in the brain 2.6 times greater than in a population with medium or low levels.
This supports the role of uric acid in increasing the risk of cerebrovascular disease and may explain the link between increased uric acid and mild cognitive impairment in older patients. There is a clear relationship between high levels of uric acid and diseases such as hypertension, type II diabetes, and metabolic syndrome. All of these conditions are known risk factors for dementia.
It is noteworthy that the average level of uric acid in the presence of an erection disorder was higher (about 12 mg / dl) than in patients with normal sexual function (about 5 mg / dl). As a result, it was found that the presence of excess content of this substance in the blood increases the risk of erectile dysfunction by almost 6 times. And an increase in uric acid levels for every 1 mg / dL is accompanied by a doubled increase in the likelihood of erection disorders.
3. Positive moments of action of uric acid
According to some researchers, an increase in urinary can have a beneficial effect on the body. In its chemical structure, uric acid is similar to trimethylated xanthine caffeine and therefore can increase mental and physical performance.
Numerous studies in the 1960s and 70s confirmed that people with hyperuricemia are more intelligent and responsive. However, uric acid does not act on adenosine receptors (which are stimulated by caffeine), most studies show a relatively small biological effect, and the socioeconomic status of the participants had a possible influence.
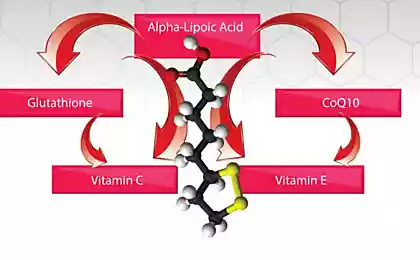
Another useful property of MK is its ability to act as an antioxidant that blocks superoxide, peroxynitrite and iron-catalyzed oxidative reactions. A number of authors suggest that elevated MK may be one of the key plasma antioxidants and prevent age-related oxidative stress, thereby contributing to life extension. Studies have shown that transfusion of uric acid in humans increases the antioxidant activity of serum and improves endothelial function.
If in general uric acid has a negative effect, then within the central nervous system it plays a completely different role. Uric acid is known as a potent neuroprotector and inhibitor of neurodegeneration and neuroinflammation. How she works there, there are different opinions. But now, in people with hyperuricemia, there is a reduced risk of neurodegenerative diseases, such as Parkinson's disease or Alzheimer's, and multiple sclerosis.
The ability of elevated uric acid levels to reduce peroxynitrite-mediated formation of nitrotyrosine indicates neuroprotective properties, which is especially important in multiple sclerosis, Parkinson's disease, stroke and other neurological diseases.
According to epidemiological studies, people with GI are much less likely to suffer from multiple sclerosis, Parkinson's disease and Alzheimer's disease, and uric acid infusion can reduce neurological manifestations obtained experimentally (for example, in experimental allergic encephalomyelitis).
High levels of urate (uric acid salts) in the blood slow the progression of Parkinson’s disease. Urates are normally contained in blood, urine and cerebrospinal fluid. These substances are powerful antioxidants that protect the body from harmful molecules - free radicals. It turned out that the participants with the highest levels of urate in the blood developed the disease more slowly.
Recent studies have shown that the beneficial effect of uric acid in these conditions is not due to its nitrothyrosine-suppressive antioxidant effect, but rather to the ability to block the blood-brain barrier or to the effect on astroglial cells.
4. The uric acid paradox.
So, if an acute increase in uric acid (uric acid is increased) has an antioxidant effect and favorably affects endothelial function, then chronic hyperuricemia, on the contrary, contributes to the development of oxidative stress and endothelial dysfunction. Perhaps this is due to various intracellular and intravascular influences of acute and chronic hyperuricemia.
Oxidative stress is a major factor in brain damage in patients with ischemic stroke. Uric acid is a potent endogenous antioxidant molecule. During experimental ischemia in rats, exogenous administration of uric acid has a neuroprotective effect, intravenous administration of uric acid is safe, prevents early decrease in uric acid levels and reduces early increase in markers of oxidative stress.
The greatest benefits from the use of uric acid were women, patients with moderately large stroke and patients with high blood glucose. Dr. Chamorro explained this fact by saying that these patients may have higher levels of oxidative stress, and uric acid is a powerful antioxidant.
Author: Andrey Beloveskin
P.S. And remember, just changing our consumption – together we change the world!
Join us on Facebook, VKontakte, Odnoklassniki
Source: www.beloveshkin.com/2015/02/blog-post_9.html
Concentrations of 5.75 mg/dL or higher for men and 4.8 mg/dL or higher for women were classified as “high normal,” meaning a certain health effect. Uric acid is elevated if its level is more than 7.0 mg / dL and is associated with an increased risk of developing gout or kidney stones.
Elevated uric acid levels
A new wave of interest in uric acid is associated with an understanding of the role of asymptomatic hyperuricemia (defined most commonly as an increase in plasma uric acid levels of 7.0 mg/dL) as a powerful, independent and modifiable risk factor for cardiovascular disease and mortality, based on data from numerous epidemiological and prospective studies.
The most common causes affecting uric acid levels are obesity, insulin resistance, metabolic syndrome, arterial hypertension, use of diuretics and low doses of acetylsalicylic acid, excessive alcohol consumption, old age, kidney failure. Among them, the leading metabolic syndrome and its components. Alcohol, impaired renal function and obesity are also associated with higher levels of uric acid.
0. Asymptomatic increase in uric acid levels.
According to the recommendations of the EULAR (European Antirheumatic League), hyperuricemia (GU) is considered an increase in uric acid (MC) of blood serum above 360 μmol / l. It often happens that you have an elevated level of uric acid, but there is no disease, this condition happens according to a number of estimates, in Belarus and the Russian Federation, one in five.
According to more modest estimates, 5–8% of the population have an asymptomatic increase in the level of MK, of which only 5–20% develop gout Over the period from 1950 to 1980 in the population, the average serum MK level increased from 5 to 6 mg / dl.
Currently, the role of hyperuricemia as an independent predictor of cardiovascular morbidity and mortality in patients with coronary heart disease, chronic and acute heart failure, arterial hypertension and prehypertension and metabolic syndrome has been proven.
Nowadays, the question becomes more and more relevant: how “harmless” is an asymptomatic increase in uric acid levels? Read about that below.
1. Linking elevated uric acid levels to insulin resistance and obesity
An increase in uric acid, along with an increase in low-density lipoproteins, is considered part of insulin resistance syndrome, which leads to cardiovascular morbidity. Insulin resistance and hyperinsulinemia can reduce renal excretion of uric acid regardless of obesity and kidney function.
It is likely that insulin increases sodium tubular reabsorption, which is accompanied by an increase in uric acid reabsorption. Insulin resistance links hypertension, hypertriglyceridemia and hyperuricemia.
However, urinary is associated with triglycerides regardless of fasting insulin levels and obesity, showing that the mechanism underlying this association only partially relates to insulin resistance and obesity.
Selective insulin resistance is characteristic of patients with arterial hypertension, and insulin has a strong sodium retention effect, which is accompanied by a decrease in renal excretion of uric acid.
Hyperinsulinemia is also able to increase the activity of the sympathetic nervous system, which can contribute to an increase in uric acid in the blood. The view that hyperuricemia may be an indicator of insulin resistance was recently confirmed by an 8-year study proving a link between UMC and insulin resistance.
Thus, hyperuricemia in patients with arterial hypertension may indicate insulin resistance, which is definitely associated with increased cardiovascular morbidity.

Uric acid increased in abdominal obesity
Elevated levels of uric acid are obviously also associated with renal vascular resistance and have an inverse dependence on renal blood flow. Uric acid levels correlate with excretion of albumins in the urine, which are precursors to the development of nephrosclerosis, and a violation of renal hemodynamics precedes impaired uric acid metabolism in patients with nephropathy. Thus, hyperuricemia in patients with arterial hypertension most likely reflects a violation of renal hemodynamics, this is a good prognostic factor.
Many studies have found that urinary levels are associated with hyperlipidemia, particularly hypertriglyceridemia. A stronger association was found with triglycerides rather than cholesterol, leading to the suggestion that triglycerides are an intermediate link between increased uric acid and increased cholesterol. There was a weak association between uric acid levels and high-density lipoproteins.
2. The connection of uric acid with atherosclerosis.
Atherosclerosis is observed in birds, while being usually asymptomatic. Birds, like primates, eat a lot of fruit and secrete uric acid. Considering models of atherosclerosis in animals that have a different metabolism often yields potentially incorrect results. For example, the famous cholesterol rabbit is often not applicable to humans at all.
Uric acid is a pro-inflammatory substance in relation to the cardiovascular system, stimulating the release of pro-inflammatory cytokines. It is suggested that there are several potential mechanisms by which uric acid may play a pathogenetic role in the development of cardiovascular morbidity or, conversely, affect clinical manifestations in patients with established atherosclerosis, but none of them have yet been confirmed.
Obviously, elevated uric acid levels enhance the oxidation of low-density lipoproteins and promote lipid peroxygenation, and are also associated with increased production of free oxygen radicals. Oxidant stress and increased oxygenation of low-density lipoproteins in the artery wall may play a role in the progression of atherosclerosis. Uric acid may be involved in platelet adhesion and aggregation. This gave rise to the hypothesis that hyperuricemia increases the risk of coronary thrombosis in patients with already existing coronary diseases.
It is assumed that the increase in uric acid reflects damage to the endothelium. Endothelial dysfunction, manifested by a decrease in endothelium-dependent vascular relaxation as a result of the action of NO, is common in patients with diabetes and arterial hypertension and plays a role in the development of atherosclerosis.
In endothelial cells, xanthine oxide is present, which is a generator of free oxygen radicals. Uric acid and xanthine oxide are elevated and are determined in much greater concentrations in vessels affected by atherosclerosis than in healthy vascular tissue. If this mechanism is correct, then an increase in uric acid may be an accurate marker of a biological phenomenon closely associated with the progression of atherosclerosis, without directly causing the development of the process of vascular damage in which xanthine oxide may be responsible.

In turn, with constant hyperuricemia, the development of arterial hypertension is associated with the development of preglomerular arteriopathy and tubulointerstitial lesion. An increase in uric acid levels stimulates the activation of the renin-angiotensin system and exacerbates endothelial dysfunction.
In addition, under the conditions of ischemia, the enzyme xanthine oxyreductase is converted to xanthine oxidase, which leads to a change in xanthine metabolism, the conversion of uric acid from an antioxidant to a prooxidant and the stimulation of oxidative stress. Hyperuricemia leads to endothelial dysfunction by inhibiting NO synthesis. This effect of uric acid is due to its prooxidant properties under conditions of altered metabolism.
Uric acid also stimulates the proliferation of smooth muscle cells of blood vessels by activating growth factors, vasoconstrictor and pro-inflammatory molecules. Thus, uric acid is not only a marker, but also an active component of the development of hypertension.
However, most importantly, in the group of patients in whom thiazide diuretics led to an increase in MK, the number of cardiovascular events was 42% higher than in the group of patients who did not have an increase in MK.
The link between hyperuricemia (increased levels of uric acid) and the risk of cardiovascular disease has been established in large epidemiological studies. The relationship of high levels of uric acid with arterial hypertension, diabetes, insulin resistance, obesity and cardiovascular diseases caused by atherosclerosis has been proved.
The National Health and Nutrition Examination Survey (NHANES I) found an independent link between hyperuricemia and increased cardiovascular mortality. As MK levels increased, the risk of death from CHD increased by 77% in men and 300% in women. An increase in MK concentration of 1 mg/dL (59.5 μmol/L) was associated with a significant increase in mortality among both men and women.
A 12-year study (PIUMA), involving more than 1,500 previously untreated patients with hypertension, also demonstrated that serum levels are a strong predictor of cardiovascular morbidity and mortality.
A study of patients with type 2 diabetes showed a significant increase in the frequency of stroke with an increase in uric acid levels. The association remained significant even after other cardiovascular risk factors were excluded. Meanwhile, the results of the Framingham study did not reveal a significant association between uric acid levels and cardiovascular morbidity.
Hyperuricemia has been found in nearly 90% of adolescents with newly diagnosed hypertension. The results of studies indicate that the correction of hieruricemia can prevent the development of cardiovascular disasters.
So what to do with an asymptomatic increase in uric acid?
It has been shown that not only sodium monourate crystals, but also soluble uric acid in asymptomatic GI can lead to an increase in the level of inflammatory mediators and induce the proliferation of vascular smooth muscle cells in vitro. Many of these “pro-inflammatory” mediators are fundamental in the pathogenesis of atherosclerotic vascular damage and its complications. Therefore, you should slightly change the diet, about this in the next article.
Researchers from Johns Hopkins Medical University (Baltimore, Maryland, USA) found that individuals with “high normal” levels of uric acid have a volume of hyperintensive white matter in the brain 2.6 times greater than in a population with medium or low levels.
This supports the role of uric acid in increasing the risk of cerebrovascular disease and may explain the link between increased uric acid and mild cognitive impairment in older patients. There is a clear relationship between high levels of uric acid and diseases such as hypertension, type II diabetes, and metabolic syndrome. All of these conditions are known risk factors for dementia.
It is noteworthy that the average level of uric acid in the presence of an erection disorder was higher (about 12 mg / dl) than in patients with normal sexual function (about 5 mg / dl). As a result, it was found that the presence of excess content of this substance in the blood increases the risk of erectile dysfunction by almost 6 times. And an increase in uric acid levels for every 1 mg / dL is accompanied by a doubled increase in the likelihood of erection disorders.
3. Positive moments of action of uric acid
According to some researchers, an increase in urinary can have a beneficial effect on the body. In its chemical structure, uric acid is similar to trimethylated xanthine caffeine and therefore can increase mental and physical performance.
Numerous studies in the 1960s and 70s confirmed that people with hyperuricemia are more intelligent and responsive. However, uric acid does not act on adenosine receptors (which are stimulated by caffeine), most studies show a relatively small biological effect, and the socioeconomic status of the participants had a possible influence.
Another useful property of MK is its ability to act as an antioxidant that blocks superoxide, peroxynitrite and iron-catalyzed oxidative reactions. A number of authors suggest that elevated MK may be one of the key plasma antioxidants and prevent age-related oxidative stress, thereby contributing to life extension. Studies have shown that transfusion of uric acid in humans increases the antioxidant activity of serum and improves endothelial function.
If in general uric acid has a negative effect, then within the central nervous system it plays a completely different role. Uric acid is known as a potent neuroprotector and inhibitor of neurodegeneration and neuroinflammation. How she works there, there are different opinions. But now, in people with hyperuricemia, there is a reduced risk of neurodegenerative diseases, such as Parkinson's disease or Alzheimer's, and multiple sclerosis.
The ability of elevated uric acid levels to reduce peroxynitrite-mediated formation of nitrotyrosine indicates neuroprotective properties, which is especially important in multiple sclerosis, Parkinson's disease, stroke and other neurological diseases.
According to epidemiological studies, people with GI are much less likely to suffer from multiple sclerosis, Parkinson's disease and Alzheimer's disease, and uric acid infusion can reduce neurological manifestations obtained experimentally (for example, in experimental allergic encephalomyelitis).
High levels of urate (uric acid salts) in the blood slow the progression of Parkinson’s disease. Urates are normally contained in blood, urine and cerebrospinal fluid. These substances are powerful antioxidants that protect the body from harmful molecules - free radicals. It turned out that the participants with the highest levels of urate in the blood developed the disease more slowly.
Recent studies have shown that the beneficial effect of uric acid in these conditions is not due to its nitrothyrosine-suppressive antioxidant effect, but rather to the ability to block the blood-brain barrier or to the effect on astroglial cells.
4. The uric acid paradox.
So, if an acute increase in uric acid (uric acid is increased) has an antioxidant effect and favorably affects endothelial function, then chronic hyperuricemia, on the contrary, contributes to the development of oxidative stress and endothelial dysfunction. Perhaps this is due to various intracellular and intravascular influences of acute and chronic hyperuricemia.
Oxidative stress is a major factor in brain damage in patients with ischemic stroke. Uric acid is a potent endogenous antioxidant molecule. During experimental ischemia in rats, exogenous administration of uric acid has a neuroprotective effect, intravenous administration of uric acid is safe, prevents early decrease in uric acid levels and reduces early increase in markers of oxidative stress.
The greatest benefits from the use of uric acid were women, patients with moderately large stroke and patients with high blood glucose. Dr. Chamorro explained this fact by saying that these patients may have higher levels of oxidative stress, and uric acid is a powerful antioxidant.
Author: Andrey Beloveskin
P.S. And remember, just changing our consumption – together we change the world!
Join us on Facebook, VKontakte, Odnoklassniki
Source: www.beloveshkin.com/2015/02/blog-post_9.html
Gadgets that simplify holiday cottage and outside the city
The stages of development of thinking at preschool age: how and what to teach the child