226
Cough guide: how to treat, how and why all syrups and potions are long overdue to throw in the trash. Save it so you don't lose it!
You feel the worst when your child is sick. But sometimes parents do reckless things. unhealthy And unnecessary for recovery. Yes, parents, even most pediatricians sin using useless drugs.

DepositPhotos
In this article we have prepared Information guidance for parents on cough-related matters. Also consider the feasibility of using drugs, which is supported by scientific data.
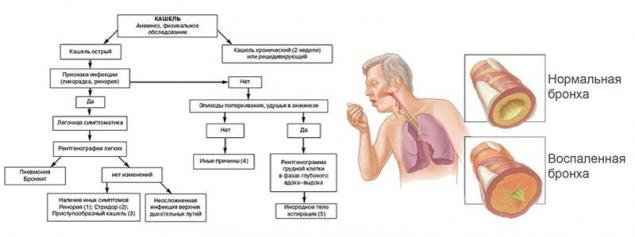
How to cure a cough in a child Let's figure out what a cough is and is it worth treating it at all? Observations of children aged 3 to 9 years show that healthy children cough up to 30 times a day! Each of us has a swelling in the air. Her overabundance causes baby-coughing. Any mechanical or inflammatory irritation of the throat, trachea, larynx, bronchi - provokes a cough. It also occurs with problems with the nervous system, when the cough center in the brain is disrupted.
Hence the conclusion - cough can be a symptom not only of respiratory diseases. Coughing is also accompanied by viral and bacterial inflammation of the respiratory tract (ARVI, bronchitis, pneumonia, whooping cough and others), allergic diseases (asthma), ENT diseases, chemical effects of the external environment, tumors of the respiratory tract.
I would like to summarize all the above and recommend the main thing - do not self-medicate, even when the disease begins with a high fever! It is not necessary to treat a cough, but a disease of which it is a symptom.
In any situation, the first thing you need to do is stop panicking, which is half the way to recovery. Let the cough bypass your loved ones, always stay healthy!
If this article was useful to you, show it to your friends on social networks, it is very important to recover correctly.

DepositPhotos
In this article we have prepared Information guidance for parents on cough-related matters. Also consider the feasibility of using drugs, which is supported by scientific data.
How to cure a cough in a child Let's figure out what a cough is and is it worth treating it at all? Observations of children aged 3 to 9 years show that healthy children cough up to 30 times a day! Each of us has a swelling in the air. Her overabundance causes baby-coughing. Any mechanical or inflammatory irritation of the throat, trachea, larynx, bronchi - provokes a cough. It also occurs with problems with the nervous system, when the cough center in the brain is disrupted.
Hence the conclusion - cough can be a symptom not only of respiratory diseases. Coughing is also accompanied by viral and bacterial inflammation of the respiratory tract (ARVI, bronchitis, pneumonia, whooping cough and others), allergic diseases (asthma), ENT diseases, chemical effects of the external environment, tumors of the respiratory tract.
- Where does the cough come from? In children's practice 80% virus accompanied by coughing. It's rhinitis, rhinosinusitis, pharyngitis, laryngitis, tracheitis, bronchitis. Note that it is normal if the child suffers from SARS up to 10 times a year.
Simultaneously with a cough in a child, you can notice such cold symptoms as nasal congestion, runny nose, high fever, chills, hoarseness, enlarged lymph nodes, chest pain during a cough attack, the appearance of clear or yellowish-green sputum. This does not mean that “everything is lost, overlooked, fell lower!” These are common symptoms of ARVI that do not require drug intervention and additional treatment.
Most SARS in compliance with the drinking regimen, temperature and humidity pass for 3 to 10 days.
By the tenth day after the onset of the disease, only 50% of children have a cold cough. In other children, the cough persists for 3-4 weeks or longer. This phenomenon is called post-infectious or post-viral cough.”
No antiviral or homeopathic pills, syrups, candles increase the chances of recovery. All of them are. Drugs with Unproven EffectivenessThere is no scientific evidence in the world regarding their therapeutic effect.
DepositPhotos
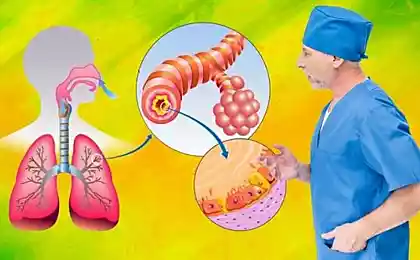
Of the entire list of pharmacy drugs that offer us for the treatment of children's cough, units can be used to treat cough. If you consider the age of 3 years, most of these drugs are potentially life-threatening.
This is especially true for cough syrups. All of them work on the principle of increasing sputum. Let’s say the child is sick, coughing, you are mucolytic syrup. Lungs and bronchi, which already suffer from an excess of sputum, begin to increase its production! The result is that the baby coughs even more. And if we add a warm room, fireplace, hot batteries - hello complications.
According to WHO recommendations, Children under 2 years are strictly forbidden to give expectorants. The risk of side effects exceeds the possible benefits. This applies to such active substances: acetylcysteine, carbocysteine, ambroxol, bromhexin, sobrerol, non-ltenexin, erdosteine and telmestein.
Without the risk of a better effect, you can achieve abundant drinking, washing the nose with saline solution and establishing optimal air parameters (room temperature up to 20 °, humidity from 40%).
Separately, drugs that depress the cough center deserve to be discussed, that is, the cough stops not because the sputum has ended, just the brains were ordered to stop its production. Medication for dry cough It is prescribed in extremely rare cases, only after confirmation of the diagnosis.
Today, there are two groups of such drugs, some affect the cough center, others weaken the signals that go to the brain from the bronchi. The use of narcotic antitussive drugs based on codeine is generally prohibited in relation to children.
DepositPhotos
“Self-acting with antitussive drugs can be very dangerous. Cough is not just an unpleasant symptom, it is the most important way for the body to cleanse the lungs. By turning off or suppressing a cough, we contribute to the fact that sputum accumulates in the lungs, which with a high degree of probability can lead to bronchitis or pneumonia, to violation of lung ventilation and other troubles.”
All sorts of "washing" camphor and eucalyptus have a good effect only on sleep, but do not reduce the frequency and strength of cough. But irritation of the skin and eyes they can cause excellent.
Abundant salivation during teething can cause coughing in young children. The saliva that drains down the back wall irritates the vocal cords and causes a reflex cough. No treatment is required. This is another fact that confirms the unjustified use of expectorants.
DepositPhotos - Urgent measures There is. diseaseThey develop very quickly and pose an immediate threat to the life of the child. Among them: pneumonia, acute bronchiolitis, croup, bacterial tracheitis, whooping cough, exacerbation of asthma, a foreign body in the respiratory tract.
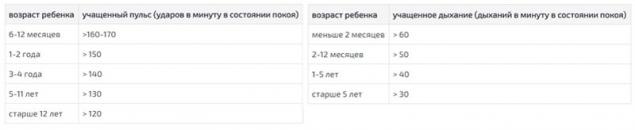
Remember the symptoms that should alert you: rapid breathing and pulse; noisy or wheezing breathing (not to be confused with “bubbling”, which is heard by the naked ear); difficulty breathing and changes in the color of the lips, skin; retraction of intercostal spaces during breathing; sudden appearance of a strong cough without other symptoms of a cold (inhalation of a foreign body); acute pain in the chest or back, lower abdomen, which increase with a deep breath; attacks of barking cough, which end in vomiting; reappearance of temperature after 48 hours of normalization.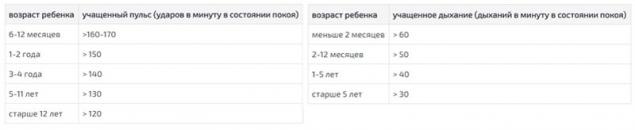
- Chronic and bacterial diseases
If the cough lasts longer than 4-8 weeks, and the child has a normal or subfebrile temperature (37.1-37.7 °), most likely there is a complex bacterial infection or exacerbation of chronic disease. Rarely, but possible cases of such diseases: whooping cough, pulmonary tuberculosis, infection with worms, ear plug, ciliary dyskinesia, cystic fibrosis, congenital lung diseases, prolonged bacterial bronchitis.
Symptoms that are most common in tuberculosis: prolonged subfebrile temperature; dry or wet cough that does not change for 8 weeks; significant weight loss; the appearance of blood in sputum. The presence of at least two symptoms from this list is a must go to the hospital!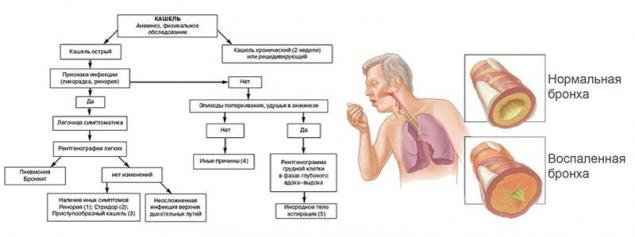
The likelihood that a child has asthma shows a short-term cough that often recurs and worsens at night or in the morning, regardless of cold episodes. It increases during physical exertion, active games, during laughter, crying or strong emotions.
It also appears after contact with a potential allergen - pets, when inhaling cold or humid air, smoke, pollen of plants, strong smells, polluted air. An important role is played by the genetic predisposition of the parents of the child to allergies. - Algorithm of actions for viral and bacterial cough If a child suddenly falls ill with all the symptoms of SARS (temperature, runny nose, general weakness), the appearance of a cough does not mean that a complication has begun. Cough can be present with absolutely pure lungs.
And this is because mucus from the sinuses (snot) drains down the throat. This is especially common in young children. It is snot that is the most common cause of coughing, if there are no problems when listening to the lungs. How do you treat this cough?
The answer is simple. Your actions: plentiful drinking, moisturizing inhaled air. If the runny nose is viral, the cough will pass by itself in 7-14 days. If bacterial, you will need an antibiotic orally (the use of antibiotics is a topic of a separate article). If allergic - specific therapy with blocking symptoms and eliminating the allergen.
DepositPhotos
Special attention deserves bronchitis, a disease that is among the five most frequent in the world. 90–95% of bronchitis is caused by viruses. Bacterial bronchitis does not occur in the first couple of days of the disease, usually it appears later as a complication.
The main symptom is a cough with or without sputum, difficulty breathing. Sometimes the doctor mentions the words "obstruction" or "obstructive bronchitis", this is when a cough is accompanied by difficulty inhaling, wheezing or wheezing. The tendency to obstruction persists in children up to 3-5 years, then passes without intervention.
Acute viral bronchitis It takes 10 to 14 days without syrups and tablets. Sometimes the cough can persist for up to a month and a half, and this is normal, since the airways should return to normal.
Acute bacterial bronchitis It requires antibiotics. Therefore, the first thing a doctor should do, if there is no improvement within 5 days of the onset of the disease, is to send for a blood test. If it shows the bacterial nature of the disease, you should take an antibacterial drug in a convenient form.
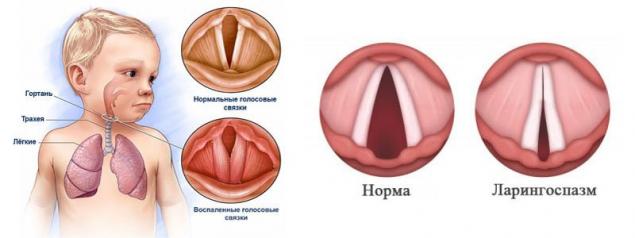
No inhalation "Dekasan", herbs and tons of "Biseptol" will not replace the correctly selected antibiotic. Up to 5 years of inhalation with any substances with a pungent smell can cause reflex laryngospasm.
Very often, viral infections are accompanied by spasm of the larynx (croup, false croup), when the larynx or trachea narrows and the child finds it difficult to breathe. This condition is also called stenosis, it is very dangerous for children at any age, because it can cause respiratory arrest.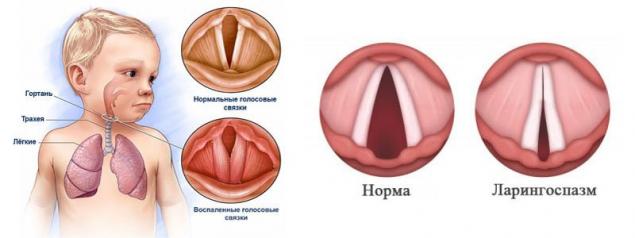
If stenosis happened suddenly, calm the child as much as possible and do not panic. If there is an increase in temperature, albeit insignificant, to 38 ° and above, give Paracetamol or Ibuprofen.
In extreme cases, humid and warm air helps to remove the spasm, which can be created in the bathroom by turning on hot water. You can also breathe cold steam from the humidifier or cool air from the street.
If there is a nebulizer at home, use it with drugs based on salbutamol or anti-inflammatory steroid hormones, it is better to check the dosage with a doctor.
If the condition does not improve or even worse, there is a change in the skin, blue hands, lips, wheezing becomes loud, immediately call an ambulance, you may need to use hormonal agents to relieve laryngeal edema.
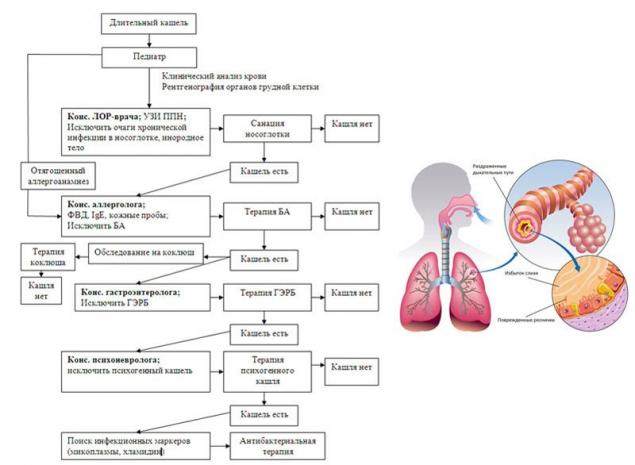
Frequent relapses of laryngospasm in a child may be a sign of narrowing of the airways not associated with infection. Consultation of a pulmonologist and an ENT doctor will be required. - Treatment for a long cough Treatment of cough that lasts more than 8 weeks should begin with the exclusion of tuberculosis, asthma. If they are not confirmed, long-term rhinosinusitis or gastroesophageal reflux disease is treated.
Children who have only one symptom are dry-cough (more than 2 weeks), it is recommended to take tests for whooping cough. If confirmed, mandatory antibacterial therapy, cool moist air, antitussive drugs are indicated, but not codeine-based. Cough provocateurs (cold, hard food, dust, cigarette smoke, physical exertion) should be avoided.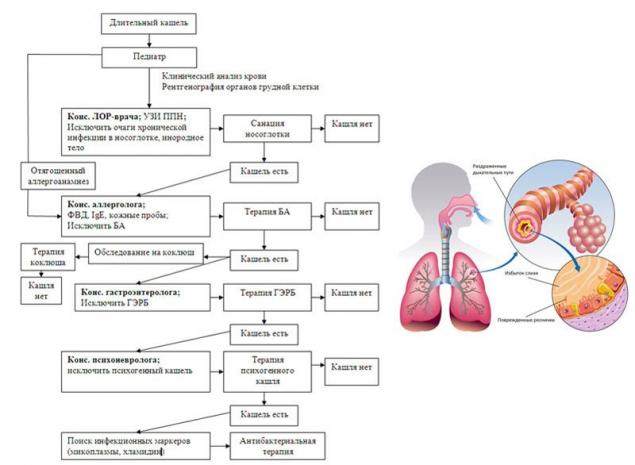
Anti-helminth therapy It is shown to children who have traces or larvae of parasites in their feces. Preventively use drugs from worms should not be, it is not candy! Also, it is not necessary to disinfect all relatives, treatment should be carried out only after confirmation of the diagnosis.
Sometimes. ear plug maybe the cause lingering, along with which there is a decrease in hearing acuity, noise in the ear, congestion or itching in the ear canal. In such cases, the child should be shown to the doctor.
If a wet cough lasts more than 4 weeks without apparent improvement and all the reasons described above are excluded, antibacterial therapy is recommended, the duration of which is set by the doctor. The drugs of the first choice are "Amoxicillin" with clavulanic acid or "Azithromycin".
There may be cases of an individual reaction of the child in the form of a cough that is caused by psychosomatic problems or sensitivity to tobacco smoke (passive smoking). - Coughing and inhalation Treatment of cough with inhalers is permissible in rare cases. Firstly, steam inhalation is prohibited for children at any age, they are useless, but the risk of burns is very high.
Application ultrasonic nebulizersIn which cold steam is produced, it is permissible to alleviate the general condition. Rules to follow: the solution for inhalation should be sterile, no "Borjomi" and "Esentuki"! Only sterile saline solution should be poured into the nebulizer, only with a sterile disposable syringe. For each inhalation, a new syringe.
DepositPhotos
If the child has obstruction, the use of special anti-asthmatic drugs is allowed. These are bronchodilators based on phenotherol, drugs that relax the muscles of the bronchi, based on salbutamol or anti-inflammatory steroid hormones.
Once again, inhalation through a nebulizer is symptomatic treatmentwhich is shown in rare cases. Its use in the first cough or sneeze is not justified, abundant drinking and cool moist air have no less efficiency than any inhalation.
With complex bronchial obstructions, the use of drugs through a spacer (balloon), but only after the age of 4-6 years, is recommended. Until this age, the use of any aerosols is prohibited due to the risk of laryngospasm. For the same reason, children under one year are not recommended to use saline solutions for the nose in a spray, only drops.
Essential oil categorically Put it in the nebulizer! It breaks into small particles under the influence of air flow. These particles settle in an even layer on the small bronchi and cause mechanical blockage, which can lead to pulmonary edema and death of the child before the arrival of the ambulance!
It is especially important to monitor the hygiene of the inhaler, which can cause bacterial or fungal infection of the airways of the child if it is used incorrectly. The glass and mask after each application should be soaked in a disinfectant solution for several minutes, after which they should be rinsed with boiled water.
DepositPhotos
I would like to summarize all the above and recommend the main thing - do not self-medicate, even when the disease begins with a high fever! It is not necessary to treat a cough, but a disease of which it is a symptom.
In any situation, the first thing you need to do is stop panicking, which is half the way to recovery. Let the cough bypass your loved ones, always stay healthy!
If this article was useful to you, show it to your friends on social networks, it is very important to recover correctly.
"Well, she's a girl..." is not an argument! This is the age at which you can pierce your child’s ears, not before.
To drive 7-8 kg of age fullness, learn to drink in the morning. It's easier to get rid of than in your youth!