244
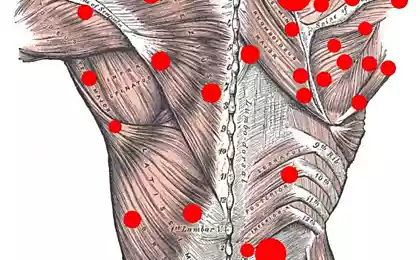
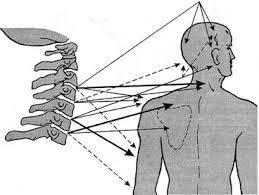
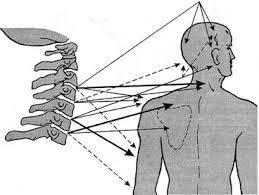
The phenomenon of reflected pain
Myofascial pain syndrome has a certain clinical picture:

Conditionally, three phases of the reverse development of myofascial pain syndrome can be distinguished:
Phase I The most acute is the constant excruciating pain from especially active trigger points. The patient can often not even explain what increases and reduces pain.
phase II Pain occurs only with movement, i.e. with increased activity of trigger points, and is absent at rest.
phase III There are only latent trigger points that do not produce pain. In this phase, the patient usually retains some dysfunction, an unstable feeling of discomfort in the corresponding area, and the trigger points retain the ability to reactivate.
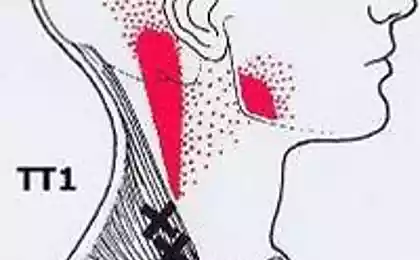
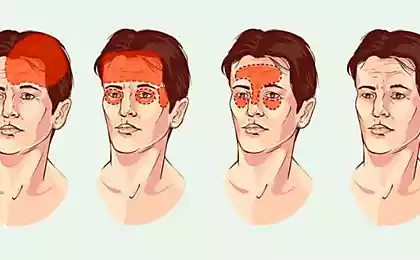
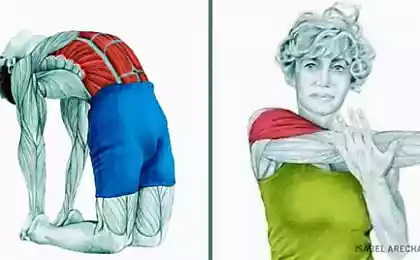
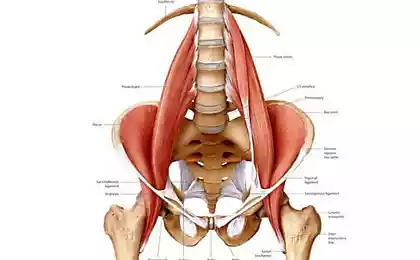
It was noted above that one of the characteristic features of pain muscle-fascial dysfunction is the phenomenon of reflected pain. Pain reflected from myofascial trigger points is usually dull and long-lasting, often felt deep within tissues; its intensity ranges from discomfort to severe and excruciating pain.
Myofascial pain reflected from a particular muscle has a specific area of spread (pattern) for that muscle. As an example, we can give areas of the face, where pain is reflected in painful muscle-fascial dysfunction of the chewing and cervical muscles.
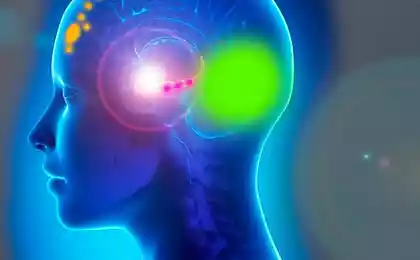
The mechanisms underlying the phenomenon of reflected pain have remained unclear for years. Currently, the concept of divergent-convergent organization of sensory flows creates the prerequisites for their understanding.
Pain in myofascial trigger points is particularly aggravated:
Myofascial pain decreases:
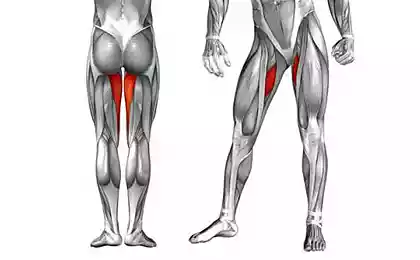
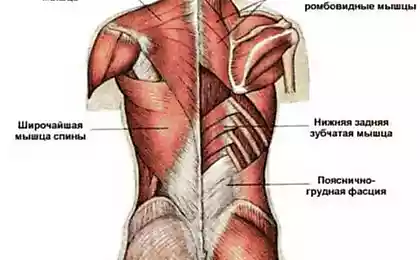
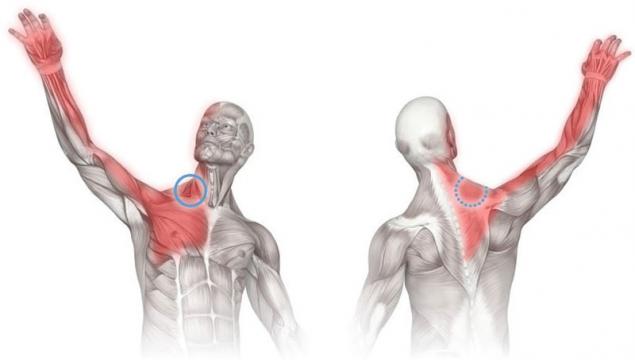
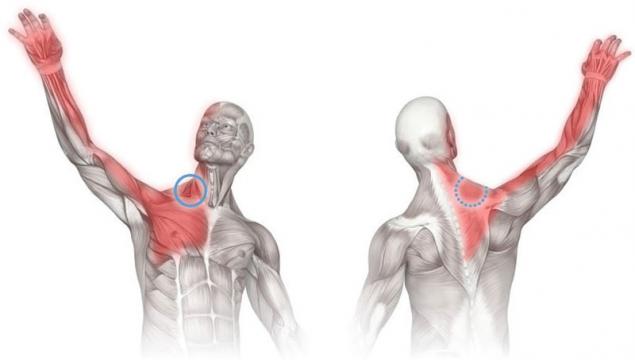
In the presence of myofascial pain syndrome, there is a restriction of mobility in combination with mild muscle weakness without atrophy of the latter. The weakness of the muscle is due to its shortening, which is consistent with Sterling’s law – length provides strength.
Limitation of the volume of movement is compensatory, thereby reducing the severity of pain.
Also interesting: 4 secrets: What the knees can tell about the health of the whole body
Tremor: When Parkinson's disease has nothing to do with it
Patients with chronic myofascial pain that lasts for many months or even longer suffer from more than just:
Source: vk.com/wall-23903469?w=wall-23903469_2860
- pain of the trigger point or points (there may be several) in the affected muscle,
- reducing the volume of movement of this muscle,
- local convulsive response when stimulating the trigger point with finger pressure or injecting a needle
- the presence of zones of reflected pain with the appearance of satellite trigger points in the same muscle, as well as in the muscles of the reflected region.

Conditionally, three phases of the reverse development of myofascial pain syndrome can be distinguished:
Phase I The most acute is the constant excruciating pain from especially active trigger points. The patient can often not even explain what increases and reduces pain.
phase II Pain occurs only with movement, i.e. with increased activity of trigger points, and is absent at rest.
phase III There are only latent trigger points that do not produce pain. In this phase, the patient usually retains some dysfunction, an unstable feeling of discomfort in the corresponding area, and the trigger points retain the ability to reactivate.
It was noted above that one of the characteristic features of pain muscle-fascial dysfunction is the phenomenon of reflected pain. Pain reflected from myofascial trigger points is usually dull and long-lasting, often felt deep within tissues; its intensity ranges from discomfort to severe and excruciating pain.
Myofascial pain reflected from a particular muscle has a specific area of spread (pattern) for that muscle. As an example, we can give areas of the face, where pain is reflected in painful muscle-fascial dysfunction of the chewing and cervical muscles.
The mechanisms underlying the phenomenon of reflected pain have remained unclear for years. Currently, the concept of divergent-convergent organization of sensory flows creates the prerequisites for their understanding.
Pain in myofascial trigger points is particularly aggravated:
- with muscle tension, mainly with isometric work,
- with passive stretching of the muscle,
- When the trigger points are compressed,
- for hypothermia.
Myofascial pain decreases:
- After a short rest,
- when applying wet hot compresses to the area of trigger points,
- with specific therapy.
In the presence of myofascial pain syndrome, there is a restriction of mobility in combination with mild muscle weakness without atrophy of the latter. The weakness of the muscle is due to its shortening, which is consistent with Sterling’s law – length provides strength.
Limitation of the volume of movement is compensatory, thereby reducing the severity of pain.
Also interesting: 4 secrets: What the knees can tell about the health of the whole body
Tremor: When Parkinson's disease has nothing to do with it
Patients with chronic myofascial pain that lasts for many months or even longer suffer from more than just:
- "Curable" pain reduces their physical activity
- impairs sleep,
- It causes depression.
- It is the cause of social maladjustment,
- In general, it significantly worsens the quality of life. published
Source: vk.com/wall-23903469?w=wall-23903469_2860
Mask with lifting effect face: 10 recipes — vibiraem!
In Argentina have found a meteorite weighing 30 tons