487
The history of the world's first cancer vaccine
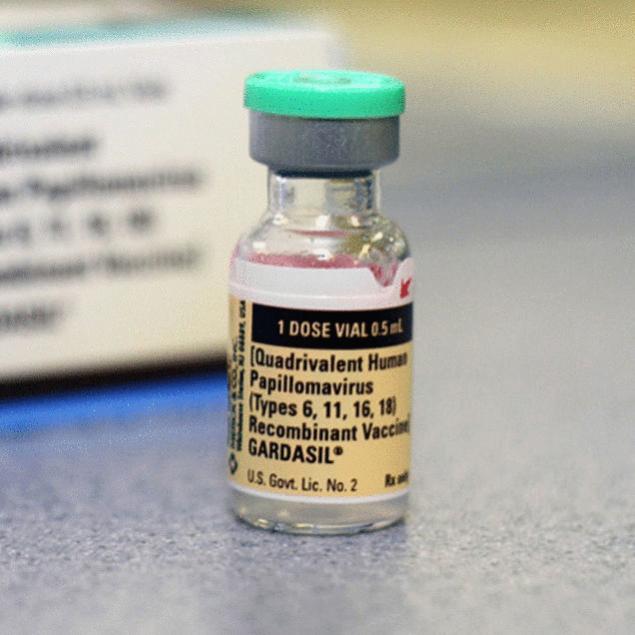
The world's first vaccine against cancer was invented not by a pharmaceutical company. Its development was funded by public organizations on two continents, brought together three universities, and the national Institute of the United States for research on cancer. This vaccine prevents infection with human papillomavirus (HPV), a disease that can lead to deadly cervical cancer. HPV is sexually transmitted and 80% of men and women develop them during their life. But thanks to a new vaccine it could forever change.
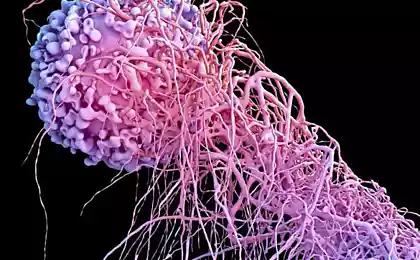
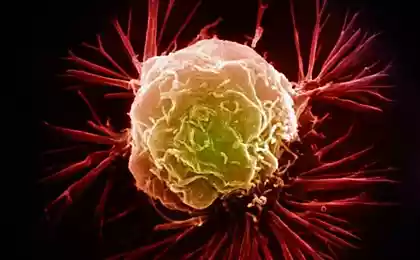
How does the vaccine against HPV HPVВакцина based on the use of virus-like particles (VLP). These particles in the HPV vaccine have the same outer protein coat (L1), and human papillomavirus, but do not contain genetic material necessary for human infection. This protein coat is the key to the mechanism of the vaccine. Thanks to shell, the particles can mimic the design of the HPV, and this structural similarity allows components of the vaccine to induce a reaction of the immune system, without putting the person at risk of infection. It is not sterilized and not dead culture of the virus, such as in the case of the flu vaccine is not a virus at all.
3 schools, 4 research groups, and at least 4 pentacosane HPV vaccine has required two decades of work. Researchers from Georgetown University won the dominant patent for HPV vaccine for their initial research in this area, however, the University's team never worked with virus-like particles. Research group at Georgetown University showed that the native structure (native form) protein shell of L1 is necessary for the formation of virus-like particles.
The U.S. patent office also considered the patent applications from the National Institute of the United States for research on cancer, University of Queensland, and the University of Rochester. Researchers from the University of Queensland has published data on two different types of protein coatings L1 and L2, and noted that these wrappers allow to assemble virus-like particles, but the thus obtained particles were fine, and properly organized. This study anticipated the publication of Georgetown University and has brought some confusion in establishing the right of a dominant patent.
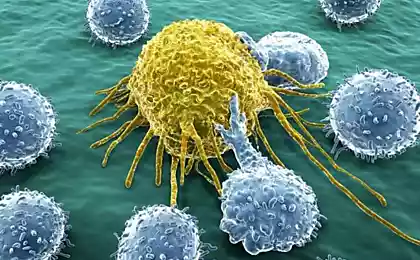
Researchers at the National Institute of the United States for research on cancer, was the first who managed to create an active virus-like particle, which was able to induce an immune response in experiments with animals. Researchers at the Institute have also determined that other teams used a mutant form of HPV L1 capsid (outer protein shell of the virus; approx. mixednews), which caused small changes in the way in which the formed particles, and thus, scientists were able to improve the process.
The team of the University of Rochester initiated the first studies that was able to launch an immune response in humans. A team of University of Queensland headed by Dr. Ian Frazer from Australia, and they sold partial patents for their discoveries concern "Merck" and the Australian company is "CSL Limited" to be able to Fund further research and clinical trials. Teams from the universities of Georgetown and Rochester was funded by grants from the National Institute for cancer research.
Perhaps these four groups worked in tandem, however, their work (and some possible academic competition) together with public funding, allows you to quickly and efficiently access and optimize virus-like particles, since most of the key discoveries that led to the creation of vaccines were done in the period between 1991 and 1993.
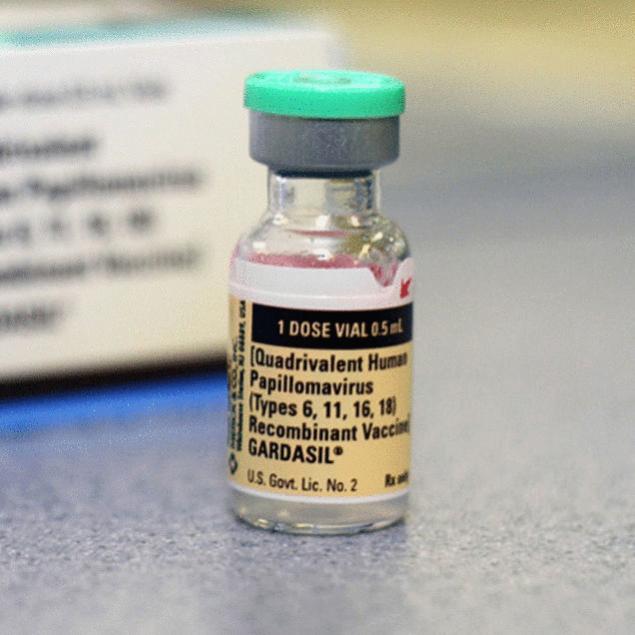
Two versions of rekawczyn vaccine "Cervarix", produced by GlaxosmithKline and certified for use in the United States in 2009, after several years of use in other parts of the world, only protects against strains HPV-16 and HPV-18, and does not protect against genital warts. Despite the lack of protection from such physical attributes of sexually transmitted diseases, one recent study by the cancer Institute showed that two of the required three injections of "Cervarix" can be enough to generate protection. This is a fairly important discovery, since the third vaccine dose should be taken six months after the initial injection, and most likely will be just skipped by the patient. On top of that, "Cervarix" has shown its effectiveness for seven years after vaccination.
The arguments against vaccinerelated about HPV vaccination of boys and young men against HPV was met with controversy. Dr. William Shaffner, Chairman of the Department of preventive medicine at Vanderbilt University of medicine, recently expressed his support for the use of the vaccine to boys and young men, emphasizing how far the original study:
My God, it's cancer of the [...] Vaccine against cancer was the dream of our youth.
You may not like injections, but it is difficult to present arguments against vaccination against papillomavirus. It is not sterilized and not a dead culture of the virus in the vaccine generally is no genetic material. HPV vaccine is a great example of how public funding and the efforts of several research universities create a powerful tandem, in the process saving many lives.
источник:mixednews.ru
Source: /users/1077
How does the vaccine against HPV HPVВакцина based on the use of virus-like particles (VLP). These particles in the HPV vaccine have the same outer protein coat (L1), and human papillomavirus, but do not contain genetic material necessary for human infection. This protein coat is the key to the mechanism of the vaccine. Thanks to shell, the particles can mimic the design of the HPV, and this structural similarity allows components of the vaccine to induce a reaction of the immune system, without putting the person at risk of infection. It is not sterilized and not dead culture of the virus, such as in the case of the flu vaccine is not a virus at all.
3 schools, 4 research groups, and at least 4 pentacosane HPV vaccine has required two decades of work. Researchers from Georgetown University won the dominant patent for HPV vaccine for their initial research in this area, however, the University's team never worked with virus-like particles. Research group at Georgetown University showed that the native structure (native form) protein shell of L1 is necessary for the formation of virus-like particles.
The U.S. patent office also considered the patent applications from the National Institute of the United States for research on cancer, University of Queensland, and the University of Rochester. Researchers from the University of Queensland has published data on two different types of protein coatings L1 and L2, and noted that these wrappers allow to assemble virus-like particles, but the thus obtained particles were fine, and properly organized. This study anticipated the publication of Georgetown University and has brought some confusion in establishing the right of a dominant patent.
Researchers at the National Institute of the United States for research on cancer, was the first who managed to create an active virus-like particle, which was able to induce an immune response in experiments with animals. Researchers at the Institute have also determined that other teams used a mutant form of HPV L1 capsid (outer protein shell of the virus; approx. mixednews), which caused small changes in the way in which the formed particles, and thus, scientists were able to improve the process.
The team of the University of Rochester initiated the first studies that was able to launch an immune response in humans. A team of University of Queensland headed by Dr. Ian Frazer from Australia, and they sold partial patents for their discoveries concern "Merck" and the Australian company is "CSL Limited" to be able to Fund further research and clinical trials. Teams from the universities of Georgetown and Rochester was funded by grants from the National Institute for cancer research.
Perhaps these four groups worked in tandem, however, their work (and some possible academic competition) together with public funding, allows you to quickly and efficiently access and optimize virus-like particles, since most of the key discoveries that led to the creation of vaccines were done in the period between 1991 and 1993.
Two versions of rekawczyn vaccine "Cervarix", produced by GlaxosmithKline and certified for use in the United States in 2009, after several years of use in other parts of the world, only protects against strains HPV-16 and HPV-18, and does not protect against genital warts. Despite the lack of protection from such physical attributes of sexually transmitted diseases, one recent study by the cancer Institute showed that two of the required three injections of "Cervarix" can be enough to generate protection. This is a fairly important discovery, since the third vaccine dose should be taken six months after the initial injection, and most likely will be just skipped by the patient. On top of that, "Cervarix" has shown its effectiveness for seven years after vaccination.
The arguments against vaccinerelated about HPV vaccination of boys and young men against HPV was met with controversy. Dr. William Shaffner, Chairman of the Department of preventive medicine at Vanderbilt University of medicine, recently expressed his support for the use of the vaccine to boys and young men, emphasizing how far the original study:
My God, it's cancer of the [...] Vaccine against cancer was the dream of our youth.
You may not like injections, but it is difficult to present arguments against vaccination against papillomavirus. It is not sterilized and not a dead culture of the virus in the vaccine generally is no genetic material. HPV vaccine is a great example of how public funding and the efforts of several research universities create a powerful tandem, in the process saving many lives.
источник:mixednews.ru
Source: /users/1077